Abstract
Background
Delirium is the most common neuropsychiatric presentation during hospitalization. In neurosurgery, studies on predisposing and precipitating risk factors for the development of delirium are rare but required for the individual risk estimation.
Methods
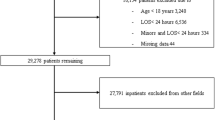
Prospective cohort study in a tertiary university center. In total, 949 neurosurgical patients, 307 with and 642 without delirium, were included. Demographic factors, neurosurgery-related, neurological, and medical clusters were tested as predictors of delirium in multiple logistic regression analyses.
Results
The incidence of delirium in this cohort of neurosurgical patients was 32.4%. Compared to patients without delirium, those with delirium were significantly older, more cognitively and neurologically impaired, transferred from hospitals and nursing homes, admitted as emergencies, longer hospitalized (16.2 vs. 9.5 days; p < 0.001), in greater need of intensive care management, and more frequently transferred to rehabilitation. Predisposing factors of delirium were stroke (OR 5.45, CI 2.12–14.0, p < 0.001), cardiac insufficiency (OR 4.59, CI 1.09–19.26, p = 0.038), cerebral neoplasm (OR 1.53, CI 0.92–2.54, p = 0.019), and age ≥ 65 years (OR 1.47, CI 1.03–2.09, p = 0.030). Precipitating factors of delirium were acute cerebral injury (OR 3.91, CI 2.24–6.83, p < 0.001), hydrocephalus (OR 3.10, CI 1.98–4.87, p < 0.001), and intracranial hemorrhage (OR 1.90, CI 1.23–2.94, p = 0.004).
Conclusions
Delirium in acute neurosurgical patients was associated with longer hospitalization. Whereas common etiologies of delirium like infections and dementia, did not predict delirium, pre-existing neurovascular and traumatic diseases, as well as surgery-related events seem important risk factors contributing to delirium in neurosurgery.


Similar content being viewed by others
Abbreviations
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- ICU:
-
Intensive care unit
- DOS:
-
Delirium Observation Screening Scale
- LOS:
-
Length of stay
- CCI:
-
Charlson Comorbidity index
- ICD:
-
International Classification of Diseases
References
Agar MR, Lawlor PG, Quinn S, Draper B, Caplan GA, Rowett D, Sanderson C, Hardy J, Le B, Eckermann S, McCaffrey N, Devilee L, Fazekas B, Hill M, Currow DC (2017) Efficacy of oral risperidone, haloperidol, or placebo for symptoms of delirium among patients in palliative care: a randomized clinical trial. JAMA Intern Med 177:34–42. https://doi.org/10.1001/jamainternmed.2016.7491
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th edition, Text Revision. Washington, DC, American psychiatric association. 124-127. 2000. (2000)
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edition. Washington, DC: American Psychiatric Association; 2013 (2013)
Budenas A, Tamasauskas S, Sliauzys A, Navickaite I, Sidaraite M, Pranckeviciene A, Deltuva VP, Tamasauskas A, Bunevicius A (2018) Incidence and clinical significance of postoperative delirium after brain tumor surgery. Acta Neurochir 160:2327–2337. https://doi.org/10.1007/s00701-018-3718-2
Burns A, Gallagley A, Byrne J (2004) Delirium. J Neurol Neurosurg Psychiatry 75:362–367
Caeiro L, Ferro JM, Albuquerque R, Figueira ML (2004) Delirium in the first days of acute stroke. J Neurol 251:171–178. https://doi.org/10.1007/s00415-004-0294-6
Caeiro L, Menger C, Ferro JM, Albuquerque R, Figueira ML (2005) Delirium in acute subarachnoid haemorrhage. Cerebrovasc Dis(Basel, Switzerland) 19:31–38. https://doi.org/10.1159/000081909
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Chen L, Xu M, Li GY, Cai WX, Zhou JX (2014) Incidence, risk factors and consequences of emergence agitation in adult patients after elective craniotomy for brain tumor: a prospective cohort study. PLoS One 9:e114239. https://doi.org/10.1371/journal.pone.0114239
Flanigan PM, Jahangiri A, Weinstein D, Dayani F, Chandra A, Kanungo I, Choi S, Sankaran S, Molinaro AM, McDermott MW, Berger MS, Aghi MK (2018) Postoperative delirium in glioblastoma patients: risk factors and prognostic implications. Neurosurgery 83:1161–1172. https://doi.org/10.1093/neuros/nyx606
Fong TG, Tulebaev SR, Inouye SK (2009) Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol 5:210–220. https://doi.org/10.1038/nrneurol.2009.24
Franco JG, Trzepacz PT, Meagher DJ, Kean J, Lee Y, Kim JL, Kishi Y, Furlanetto LM, Negreiros D, Huang MC, Chen CH, Leonard M, de Pablo J (2013) Three core domains of delirium validated using exploratory and confirmatory factor analyses. Psychosomatics 54:227–238. https://doi.org/10.1016/j.psym.2012.06.010
Girard TD, Exline MC, Carson SS, Hough CL, Rock P, Gong MN, Douglas IS, Malhotra A, Owens RL, Feinstein DJ, Khan B, Pisani MA, Hyzy RC, Schmidt GA, Schweickert WD, Hite RD, Bowton DL, Masica AL, Thompson JL, Chandrasekhar R, Pun BT, Strength C, Boehm LM, Jackson JC, Pandharipande PP, Brummel NE, Hughes CG, Patel MB, Stollings JL, Bernard GR, Dittus RS, Ely EW (2018) Haloperidol and ziprasidone for treatment of delirium in critical illness. N Engl J Med. https://doi.org/10.1056/NEJMoa1808217
Inouye SK (1998) Delirium in hospitalized older patients. Clin Geriatr Med 14:745–764
Inouye SK (2006) Delirium in older persons. N Engl J Med 354:1157–1165. https://doi.org/10.1056/NEJMra052321
Inouye SK, Charpentier PA (1996) Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. Jama 275:852–857
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113:941–948
Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. Lancet (London, England) 383:911–922. https://doi.org/10.1016/s0140-6736(13)60688-1
Kahn RL, Goldfarb AI, Pollack M, Peck A (1960) Brief objective measures for the determination of mental status in the aged. Am J Psychiatry 117:326–328. https://doi.org/10.1176/ajp.117.4.326
Kozak HH, Uguz F, Kilinc I, Uca AU, Serhat Tokgoz O, Akpinar Z, Ozer N (2017) Delirium in patients with acute ischemic stroke admitted to the non-intensive stroke unit: incidence and association between clinical features and inflammatory markers. Neurol Neurochir Pol 51:38–44. https://doi.org/10.1016/j.pjnns.2016.10.004
Matano F, Mizunari T, Yamada K, Kobayashi S, Murai Y, Morita A (2017) Environmental and clinical risk factors for delirium in a neurosurgical center: a prospective study. World neurosurgery 103:424–430. https://doi.org/10.1016/j.wneu.2017.03.139
Naidech AM, Beaumont JL, Rosenberg NF, Maas MB, Kosteva AR, Ault ML, Cella D, Ely EW (2013) Intracerebral hemorrhage and delirium symptoms. Length of stay, function, and quality of life in a 114-patient cohort. Am J Respir Crit Care Med 188:1331–1337. https://doi.org/10.1164/rccm.201307-1256OC
National Institute for Health and Clinical Excellence.(2010) Delirium: diagnosis, prevention and management. 2010.
Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM (2016) Antipsychotic medication for prevention and treatment of delirium in hospitalized adults: a systematic review and meta-analysis. J Am Geriatr Soc 64:705–714. https://doi.org/10.1111/jgs.14076
Organization WH (1992) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization, Geneva
Park SH, Sohn MK, Jee S, Yang SS (2017) The characteristics of cognitive impairment and their effects on functional outcome after inpatient rehabilitation in subacute stroke patients. Ann Rehabil Med 41:734–742. https://doi.org/10.5535/arm.2017.41.5.734
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the heart failure association (HFA) of the ESC. Eur J Heart Fail 18:891–975. https://doi.org/10.1002/ejhf.592
Qu J, Chen Y, Luo G, Zhong H, Xiao W, Yin H (2018) Delirium in the acute phase of ischemic stroke: incidence, risk factors, and effects on functional outcome. J Stroke Cerebrovasc Dis : Off J National Stroke Assoc 27:2641–2647. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.05.034
Sauvigny T, Mohme M, Grensemann J, Duhrsen L, Regelsberger J, Kluge S, Schmidt NO, Westphal M, Czorlich P (2018) Rate and risk factors for a hyperactivity delirium in patients with aneurysmal subarachnoid haemorrhage. Neurosurg Rev. https://doi.org/10.1007/s10143-018-0990-9
Schuurmans MJ, Shortridge-Baggett LM, Duursma SA (2003) The delirium observation screening scale: a screening instrument for delirium. Res Theory Nurs Pract 17:31–50
Siddiqi N, Harrison JK, Clegg A, Teale EA, Young J, Taylor J, Simpkins SA (2016) Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev 3:Cd005563. https://doi.org/10.1002/14651858.CD005563.pub3
Stillman MJ, Rybicki LA (2000) The bedside confusion scale: development of a portable bedside test for confusion and its application to the palliative medicine population. J Palliat Med 3:449–456. https://doi.org/10.1089/jpm.2000.3.4.449
Tanaka M, Tani N, Maruo T, Oshino S, Hosomi K, Saitoh Y, Kishima H (2018) Risk factors for postoperative delirium after deep brain stimulation surgery for Parkinson disease. World Neurosurg 114:e518–e523. https://doi.org/10.1016/j.wneu.2018.03.021
Taulbee LR, Folsom JC (1966) Reality orientation for geriatric patients. Hosp Community Psychiatry 17:133–135
Trzepacz PTB, W.; Franklin, J.; Levenson, J.; Martini, R.;, Wang, P. (1999) Practice guideline for the treatment of patients with delirium. Am Psychiatric Assoc Am J Psychiatry 156:1–20
van den Boogaard M, Schoonhoven L, van der Hoeven JG, van Achterberg T, Pickkers P (2012) Incidence and short-term consequences of delirium in critically ill patients: a prospective observational cohort study. Int J Nurs Stud 49:775–783. https://doi.org/10.1016/j.ijnurstu.2011.11.016
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M (2007) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann Intern Med 147:W163–W194
Vasilevskis EE, Han JH, Hughes CG, Ely EW (2012) Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol 26:277–287. https://doi.org/10.1016/j.bpa.2012.07.003
Wang J, Ji Y, Wang N, Chen W, Bao Y, Qin Q, Xiao Q, Li S (2018) Risk factors for the incidence of delirium in cerebrovascular patients in a neurosurgery intensive care unit: a prospective study. J Clin Nurs 27:407–415. https://doi.org/10.1111/jocn.13943
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery general
Rights and permissions
About this article
Cite this article
Zipser, C.M., Deuel, J., Ernst, J. et al. The predisposing and precipitating risk factors for delirium in neurosurgery: a prospective cohort study of 949 patients. Acta Neurochir 161, 1307–1315 (2019). https://doi.org/10.1007/s00701-019-03927-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-03927-z