On Call: The Newsletter of the Alliance of Specialty Medicine
Winter 2023

Representatives of the Alliance of Specialty Medicine met virtually in early January to discuss their federal agenda for the newly convened 118th Congress. The specialty coalition also welcomed its newest member, the Society of Interventional Radiology (SIR).
to discuss their federal agenda for the newly convened 118th Congress. The specialty coalition also welcomed its newest member, the Society of Interventional Radiology (SIR).
The addition of SIR brings the Alliance membership up to 16 national medical specialty societies and adds 8,000 more doctors’ voices for a specialty docs’ total headcount of well over 100,000 specialty physicians nationwide. You can read more about SIR in a feature story in this newsletter.
Since its founding, the Alliance has focused on providing greater access to specialty care. With that focus in mind, the Alliance will renew its push to create a stable payment system for its Medicare providers this year. For several years, Medicare reimbursement rates have declined due to the budget neutrality requirement in the Medicare Physician Fee Schedule (MPFS) and the lack of an inflation adjustment in the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). Specialty practices across the nation cannot survive this trend of year-over-year cuts and will again press Congress for oversight hearings and reforms to MACRA as well as fairer treatment under the MPFS.
Patient access to specialty care is also hampered by abuses of prior authorization and step therapy requirements. These measures, crafted initially to save money in the healthcare system, have instead become arbitrary methods for insurance providers to deny care and protect their own profits. While the Alliance was pleased to participate in a roundtable discussion on prior authorization reform sponsored by the Centers for Medicare & Medicaid Services (CMS), we will continue to advocate for passage of the Improving Seniors’ Timely Access to Care Act and the Safe Step Act in the 118th Congress.
This year, the Alliance will also remain active in working with federal healthcare agencies to relieve regulatory burdens on specialty practices. The Alliance responded to proposals outlined in a recent rule addressing Affordable Care Act (ACA) or Exchange plans. In their formal comments, the specialty group highlighted considerable access to care challenges facing consumers in ACA plans due to flawed network adequacy criteria that fail to account for all specialists, and particularly subspecialists. To address the problem, the Alliance urged CMS to revise its requirements so all specialists and subspecialists are considered and recommended establishing new plan-level quality measures to incentivize robust networks.
Paralleling its legislative push to reform prior authorization, The Alliance of Specialty Medicine also sent formal comments to the Centers for Medicare and Medicaid Services (CMS) urging the agency to finalize proposed policies that would meaningfully improve utilization management (UM) and plan marketing in the Medicare Advantage (MA) program. Specific to utilization management, the specialists highlighted the importance of the reforms for specialty physicians and their patients, who are often subject to prior authorizations and other UM tactics, and asked the agency to expand its proposals to Part D. In addition, the Alliance urged CMS to rescind its step therapy policies in light of the proposed changes, and at a minimum, revise the guidance, so it’s consistent with the continuity of care proposals.
More recently, CMS introduced its Advancing Interoperability and Improving Prior Authorization proposed rule, which proposes additional requirements on payers, including MA plans, to reduce provider burden and improve care coordination. This rule would make important updates to ensure patients and providers have more immediate access to patient data held by payers, including prior authorization information, and ensure that payers adopt standardized electronic prior authorization processes that are more transparent and timely. The Alliance is generally supportive of this rule and is currently working on a response to CMS.
 In January, The Alliance of Specialty Medicine (Alliance) participated in an in-person roundtable discussion on reforming prior authorization in federally-sponsored healthcare programs. The panel was convened by Centers for Medicare & Medicaid Services (CMS) Administrator Chiquita Brooks-LaSure, and U.S. Surgeon General Vice Admiral Vivek H. Murthy, MD, as the Biden Administration looks to remedy documented abuses in the prior authorization program and ensure patients’ timely access to medically necessary care.
In January, The Alliance of Specialty Medicine (Alliance) participated in an in-person roundtable discussion on reforming prior authorization in federally-sponsored healthcare programs. The panel was convened by Centers for Medicare & Medicaid Services (CMS) Administrator Chiquita Brooks-LaSure, and U.S. Surgeon General Vice Admiral Vivek H. Murthy, MD, as the Biden Administration looks to remedy documented abuses in the prior authorization program and ensure patients’ timely access to medically necessary care.
The Alliance specialty physicians who participated in today’s roundtable echoed these findings.
Eugene Y. Rhee, MD, MBA, public policy chair of the American Urological Association, said, “Prior authorization is a barrier to care that profoundly harms patients. The AUA applauds CMS for the opportunity to participate in today’s dialogue about how we can remove this barrier so that patients can get the care they need when they need it. Ongoing communication is key to ensuring CMS understands and addresses the daily challenges that physicians and their patients face.”
Shivan Mehta, MD, MBA, a gastroenterologist who attended the meeting for the Alliance, noted, “We know that health disparities exist in many GI conditions and diseases, and prior authorization only exacerbates this problem. The solutions that HHS is offering will make a difference in ensuring patients can get the care they need when they need it.”
Also attending for the Alliance was Katie O. Orrico, Esq., SVP for health policy and advocacy for the American Association of Neurological Surgeons and Congress of Neurological Surgeons, who added, “It’s long past the time for CMS to hold health plans accountable for unconscionable delays and denials of care. The Alliance looks forward to CMS finalizing these proposals, which will eliminate care delays, patient harms, and practice hassles contributing to physician burnout.”
The Alliance has been a long-time proponent of reform to prior authorization. Unfortunately, the program has devolved into a cumbersome process that requires physicians to obtain pre-approval for medical treatments or tests before rendering care to their patients. The process for obtaining approval is lengthy and typically requires physicians or their staff to spend the equivalent of two or more days each week negotiating with insurance companies — time that would better be spent taking care of patients. Patients experience significant barriers to medically necessary care due to prior authorization requirements for items and services that are eventually routinely approved.
The Alliance recently released a survey of its physician members about prior 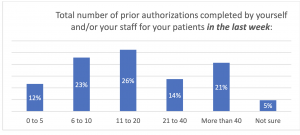 authorization and other utilization review practices. Respondents overwhelmingly indicated that the use of prior authorization (PA) has increased in the last five years across all categories of services and treatments:
authorization and other utilization review practices. Respondents overwhelmingly indicated that the use of prior authorization (PA) has increased in the last five years across all categories of services and treatments:
The Biden Administration recently proposed several regulations to improve prior authorization:
The Alliance is currently reviewing these proposals and will submit written comments. In addition, the Alliance is also advocating for statutory reforms, including the bipartisan Improving Seniors’ Timely Access to Care Act (H.R. 3173/S. 3018), which closely aligns with the provisions included in the CMS prior authorization proposals. The House bill had 327 cosponsors and passed unanimously by voice vote. The Senate bill had 53 bipartisan cosponsors, but unfortunately, the bill was not included in the Consolidated Appropriations Act of 2023 at the end of last year.

The Alliance of Specialty Medicine is proud to welcome its newest member, the Society of Interventional Radiology (SIR).
SIR is the voice for the interventional radiology community, representing more than 8,000 practicing interventional radiology physicians, trainees, medical students, scientists, and clinical associates, including physician assistants, nurse practitioners, radiologic technologists, and paramedical professionals.
SIR offers members support throughout their careers by developing tools and education that further their practices. SIR also provides mentorship and recruitment programs to attract the best and brightest talent from all backgrounds to advance the specialty and to better represent the patient population IRs serve.
Dedicated to improving patient care through minimally invasive, image-guided therapies, interventional radiologists work collaboratively with other specialties to treat conditions across the body, including cardiovascular and venous disease, cancer, kidney disease, stroke, gynecological disease, urological disease, chronic pain and more.
Through its research arm, SIR Foundation, the society funds research into the development and enhancement of innovative therapies from inception to mature clinical application.
SIR is pleased to be a part of the Alliance of Specialty Medicine and looks forward to collaborating with other member societies to improve healthcare policies and ensure patients everywhere have access to the care they need.
For more information about the Society of Interventional Radiology and SIR Foundation, visit sirweb.org.
 The 117th Congress ended on a harsh note for Medicare providers. Despite a fierce advocacy campaign asking Congress to forestall a scheduled 4.47% cut to providers set out by the Medicare Physician Fee Schedule (MPFS), Congress responded by failing to address the cut fully and instead pushed only a 2.5% one-year adjustment, resulting in an over 2% overall cut to physicians in 2023.
The 117th Congress ended on a harsh note for Medicare providers. Despite a fierce advocacy campaign asking Congress to forestall a scheduled 4.47% cut to providers set out by the Medicare Physician Fee Schedule (MPFS), Congress responded by failing to address the cut fully and instead pushed only a 2.5% one-year adjustment, resulting in an over 2% overall cut to physicians in 2023.
The cuts to Medicare providers were not unanticipated. In fact, many physician groups like the Alliance of Specialty Medicine (Alliance) had been warning Congress all year. This is due to the fact that under statute, the Medicare Physician Fee Schedule is subject to a statutory budget neutrality requirement. This is compounded by the fact that, under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), physician payments are subject to a conversion factor that does not adjust for inflation. These factors, plus other weaknesses in MACRA, such as its lack of quality measures for many specialty and sub-specialty practices and expiring incentives to create and participate in alternative payment models (APMs) mean that most specialty providers are now faced with year-over-year cuts.
In addition to the unbalanced treatment specialists received under MACRA, the provider community had to brace for a 4% hit due to the Statutory Pay-As-You-Go Act of 2010 (P.L. 111-139), which was triggered by the COVID-19 relief package passed in 2021. And finally, providers had to absorb the full effect of a 2% Medicare sequester cut mandated by the Budget Control Act of 2011 (P.L. 112-25), which came out of the debt ceiling crisis over a decade ago. All told, physicians serving Medicare patients may have to face upwards of 10% in cuts every year due to outdated healthcare laws like MACRA or as a result of federal spending negotiations in which physicians are merely bystanders. It has been well documented to Congress that despite enduring the same inflation rates as hospitals and other medical facilities, physicians are threatened with cuts rather than positive adjustments that account for rising inflation.
The layers of cuts imposed on physicians create immense challenges in maintaining solvent practices, retaining and recruiting qualified staff, and ensuring patient access to health care. Because of the year-over-year reductions in Medicare reimbursements over the past several years, more and more physician practices have been forced to take drastic measures, including limiting the number of Medicare patients they see, consolidating with larger hospital or health care systems, which increases costs to the Medicare program, or worse, retiring early and permanently closing their doors.
Anthony M. DiGiorgio, DO, MHA, and Praveen V. Mummaneni, MD, MBA
Electronic health records (EHRs), once promised to revolutionize healthcare, are becoming a burden. We audited the EHR logs at our institution, the University of California San Francisco, to examine our neurosurgery residents’ work and better understand the benefits and burdens. The results shocked us: the on-call residents spent 20 hours logged into the EHR over a single shift. When we shared these results with the residents, they weren’t surprised. They feel that EHR burden every day.
The Promise and Disappointment of EHRs
The EHR has plenty of benefits. Gone are the days of hunting for films in the radiology basement, searching the floors for that missing chart, or deciphering the infamously bad doctor handwriting. For patients who have a usual place of care, having quick access to their past records is valuable.
 We considered whether perhaps this busywork had been replaced by more efficient EHR workflows. To see if this was the case, we examined what tasks the residents were doing when they were interacting with certain areas of the EHR. This “active time” (any time they spent moving the mouse or clicking the keyboard while in a patient chart) totaled 9 hours per shift but excluded computer activities outside of patient charts, most notably imaging review. This active time log revealed several inefficiencies, such as a daily average of 45 minutes spent searching for orders, reconciling orders, and navigating order decision support tools. This deep dive showed us that the scut work of old has been replaced with a worse EHR burden.
We considered whether perhaps this busywork had been replaced by more efficient EHR workflows. To see if this was the case, we examined what tasks the residents were doing when they were interacting with certain areas of the EHR. This “active time” (any time they spent moving the mouse or clicking the keyboard while in a patient chart) totaled 9 hours per shift but excluded computer activities outside of patient charts, most notably imaging review. This active time log revealed several inefficiencies, such as a daily average of 45 minutes spent searching for orders, reconciling orders, and navigating order decision support tools. This deep dive showed us that the scut work of old has been replaced with a worse EHR burden.
Our program is not unique in this regard. Surgery residents spend nearly eight months of their 5-year training on the EHR. Residents routinely take EHR work out of the hospital, completing up to a third of it from home. Non-surgical residents have it even worse, spending around 40% of their time on the EHR and only 12% of their time on direct patient care. Over 90% of residents say that documentation obligations are excessive and that they take away from time with patients.
The EHR burden doesn’t just affect residents. It takes a trauma surgery attending 73 full 24-hour daysto complete the required documentation for one year of billing alone. In ambulatory practices, physicians spend 2 hours on the computer for every 1 hour of patient time. EHR use is linked to physician burnout, a problem that is costing billions of dollars in the U.S.
Many of the inefficiencies we found come from Medicare regulations. The appropriate use criteria program is a good example. This was developed to reduce the unnecessary imaging ordered by physicians. When ordering a CT or MRI, the physician must click a few boxes to ensure the order is appropriate for the diagnosis. In our EHR audit, we found this added just a few minutes of computer time to the residents’ days. However, there’s no evidence that this regulation reduces unnecessary imaging. We believe it to be completely unnecessary. Many more regulations add a few minutes here and a few minutes there. It’s death by 10,000 clicks.
Steps to Relieve the Burden
Systematic identification of these inefficiencies is necessary to eliminate them. Our study, with its granular breakdown of EHR tasks, was just a start. There are many regulations around billing, coding, value-based reimbursement, and physician order entry that are adding to the EHR burden. Adding these numerous regulations was easy — identifying and eliminating them will be difficult. The Centers for Medicare & Medicaid Services “Patients Over Paperwork” initiative was a good start, as it reduced some of the documentation requirements for physician notes. That effort should be continued.
Some of the inefficiencies come from the EHR itself. Physicians often have little say in which EHR is selected and how it is set up. However, in physician-owned hospitals where doctors have more input, their satisfaction with the EHR was improved, and they reported more positive perceptions of time spent on documentation. Reversing the virtual ban on physician-owned hospitals will give physicians more say in the purchasing of an EHR, shifting the market towards those that reduce the computer burden.
Of course, increasing advanced practice provider support helps offload the remaining EHR tasks. The Accreditation Council for Graduate Medical Education (ACGME) has encouraged this. However, mindless administrative tasks should be eliminated, not simply transferred to other employees. This shifting burden explains why healthcare must employ increasingly more workers to care for the same number of patients. Advanced practice providers don’t want to be saddled with mindless administrative tasks, either.
What doesn’t help are mandatory wellness programs, doctor appreciation days, or EHR training sessions. In fact, our data showed no improvement in EHR efficiency as trainees became more experienced. The problem comes not from a lack of mental fortitude, wellness, or ambition. It’s built into the system.
Conclusions
As neurosurgeons, we should advocate for policies that decrease administrative burdens. It is detracting from our trainees’ educational experience. Healthcare costs are increasing because of the inefficiencies that come with EHRs. We must be aware of this to protect our residents and our industry. Continued involvement in advocacy is needed to reverse the ever-increasing EHR burden.
Anthony M. DiGiorgio, DO, MHA, is an assistant professor in the Department of Neurological Surgery at the University of California San Francisco and affiliated faculty at the Institute for Health Policy Studies. Praveen V. Mummaneni, MD, MBA, is the Joan O’Reilly Endowed Professor and vice-chair of the Department of Neurological Surgery at the University of California San Francisco. This article was initially published in MedPage Today.