The price of a drug crucial to prevent tuberculosis is to be slashed by two-thirds in a deal that could stop millions from developing the disease.
TB is the leading cause of death from infectious disease worldwide, killing 1.5 million people a year, according to the latest World Health Organization (WHO) global TB report.
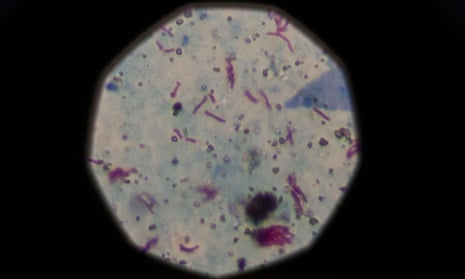
An estimated 1.7 billion people, a quarter of the world’s population, are infected by TB but have no symptoms and are not contagious. Most do not know they are infected. Access to the antibiotic, rifapentine, would stop this “latent” TB from becoming active.
Without treatment, 5% to 10% of people with latent TB – up to 170 million people globally – will develop the disease, which can be passed from person to person.
The price drop, negotiated on a volume basis by Unitaid, the Global Fund to Fight Aids, Tuberculosis and Malaria, and the pharmaceutical company Sanofi, means the drug can be used in 100 low- and middle-income countries.
Effective prevention will be a “game-changer” in eliminating TB, according to Unitaid’s executive director, Lelio Marmora. Available to those who could afford it since 2017, rifapentine has, until now, been “completely unaffordable” in developing countries. “This agreement will help transform political commitment to tangible action,” he said.
Affordability of medicines is an issue affecting countries worldwide. In England, a standoff over the price of the cystic fibrosis drug Orkambi finally ended last week.
Today, only 1.8 million people are on preventive treatment for TB. Last year at the UN, heads of state agreed a target of 30 million people by 2022. That jump looks more achievable now that the price of a three-month course of rifapentine will drop from approximately $45 (£35) to $15 for public health services in poorer countries.
Last month, donors pledged more than $14bn to replenish the Global Fund for the next three years, the largest amount raised for a multilateral health organisation. But demands on these funds are growing.
Peter Sands, the Global Fund’s executive director, said that enabling people to access the treatment would be doubly effective, keeping them healthy and therefore helping to “build more stable and prosperous communities”.
Those living with HIV are up to 37 times more likely to be affected by TB.
Until now, preventive treatment took from six to 36 months and uptake was poor. Using rifapentine shortens the care to 12 weekly doses in combination with another drug, isoniazid. Research has found that patients are much more likely to finish shorter treatments.
The WHO recommends this treatment for people living with HIV and those of any age who have had contact, for example by living in the same household, with confirmed TB cases.
Tereza Kasaeva, director of the WHO’s global TB programme, called the deal a “significant development” and said: “We hope that countries with the highest TB burdens can benefit. Continued efforts to make medicines more affordable and patient-friendly will facilitate national TB and HIV programmes quicken their pace to scale up preventive treatment services.”
South Africa, a country with high rates, plans to roll out the new treatment. The country’s minister of health, Zweli Mkhize, said: “Hundreds of thousands of vulnerable people can be initiated on this new treatment regimen starting next year, thanks to this price agreement.”
India, where more people are affected by TB than in any other country, has set a target to eliminate TB by 2025. More affordable rifapentine should help more than 1 million people.
Jon Fairest, Sanofi’s vice-president for external affairs Africa, Eurasia and Middle East, believes this is a “sustainable commercial approach” that will widen access to the “new standard of care for latent tuberculosis infection”.
Unitaid and partners are negotiating a generic supply of the drug for 2020.
Another development announced this week is a new treatment for people with extremely drug resistant TB (XDR-TB).
The drug pretomanid has recently been approved by the US Food and Drug Administration for a six-month course. This new treatment, which in combination with two other drugs, bedaquiline and linezolid, is known as BPal, reduces the time needed to tackle drug-resistant TB and is also more effective. Previous treatments typically lasted at least two years.
Mel Spigelman, president and CEO of the TB Alliance, which developed the new treatment, said it is the first to win regulatory approval anywhere, although he cautioned that “the job is not done until the medicine gets into the hands of the patients who need it”.
This week, the Global Drug Facility announced that the drug will be available for $2 a day to 140 countries with the highest incidence.
The cost of all three drugs will be roughly $1,000 for a full course. According to the Stop TB Partnership, previous treatments cost up to $8,000. MSF has called for bedaquiline to be reduced to no more than $1 a day for those who need it.
Sharonann Lynch, HIV & TB policy adviser for MSF’s access campaign, said: “It’s inexcusable that drug corporations continue to put profits over people’s lives”.
A new vaccine to prevent TB, under development by GlaxoSmithKline, is being watched with “cautious optimism”. A three-year clinical trial has shown sustained protection against tuberculosis of the lungs, a particularly aggressive form, and will now move to the next phase.