Advertisement
Advertisement
January/February 2022
Think Differently to Innovate Cardiovascular Care
Expand innovation and creativity at your organization.
What is innovation? Everyone is familiar with the notion as our daily lives depend on it. The way you are reading this article right now is the result of a long historical series of innovations: the wine screw that inspired the Gutenberg press, which changed the world’s access to written material; the Jacquard Loom that led to the conceptual mechanisms behind data processing leading to the computer; Tim Berners-Lee’s tool for scholars that evolved into the internet.
The word innovation is everywhere. In fact, most organizations’ mission statements would not be complete without its mention, which suggests that innovation is highly valued universally. It’s a societal expectation that businesses embrace innovation, from leadership to their employees, to provide value to their customers. This is especially true in the health care industry.
Although we are familiar with the concept of innovation, it can be difficult to define what it is and the role it plays in health care. Innovation is like the color yellow—you know it when you see it but it’s difficult to define. Experts have yet to agree on a single definition. However, despite the variety in answers, key elements tie the definitions together. Understanding these elements will equip you to recognize why certain innovations become successful and help unlock your innovator mindset.
ELEMENTS OF INNOVATION
Paradigm Shifts in Health Care
Innovation is typically seen as “a new invention, technology, process, or idea.” Although this definition isn’t wrong, it is limiting. Innovation is something that’s different; it’s a pattern interrupt, a break from the status quo, something that is new or with an essence of novelty to it. Novelty doesn’t necessarily mean that the innovation never existed before—in fact, innovation thrives on reinventing or reusing the old, in which case the novelty is in its creative, new application. The word innovation originates from the Latin word meaning “to renew.”
The addition of value is also an essential defining component of innovation. People can generate creative solutions to a problem, but their solution may fail to add value. Innovation requires action; although it starts with an idea, it must lead to action. Innovation can take form in things, processes, and models. Things are defined as technology, devices, and products; processes are the development of new programs and services, or how something is made; and models can be a new framework for delivering a service.
Perhaps the most defining element of genuine innovation is that it’s discontinuous, which means it’s a paradigm shift. Innovation represents a nonincremental difference, a break from what has come before. This distinguishes innovation from other ways of making things better, such as incremental, continuous improvement. In health care, we are closely familiar with the concept of continuous improvement. Process improvement and quality initiatives often center around incremental changes of improvement along a linear trajectory. Common examples include the improvement around handwashing compliance, cath lab utilization, radiation exposure, falls, and length of stay. An example of innovation—a discontinuous change—includes the invention of the defibrillator, which made it possible to save the lives of patients with ventricular fibrillation, a fatal condition prior to the defibrillator’s invention. Angioplasty is another example, first successfully accomplished by Andreas Gruentzig, MD, in 1977. This breakthrough gave rise to the subspecialty of interventional cardiology, which in turn has led to a plethora of innovations to treat cardiovascular diseases and conditions with minimally invasive procedures.1
Change Your Frame to Innovate Health Care
How do you create the ideas that could result in innovation? A frame shift, another fundamental element of innovation, is required to achieve a paradigm shift. A frame shift is essentially thinking differently. This requires seeing and understanding the world in a new way, which exercises our mind’s imaginative and creative abilities. Thinking differently is the mind’s vehicle to overcoming blind spots and cognitive biases, such as functional fixedness that hinders our ability to conceptualize other ways to use an object aside from its traditional usage.
The way forward to a brighter future is in thinking differently and doing differently, and innovation is the answer. We must approach a problem with a new frame of thinking and understanding about what we are trying to achieve. In early 2022, we continue to find ourselves in a health care crisis, with the pain points experienced prior to 2019 magnified by the COVID-19 pandemic. Extreme states and adverse conditions, such as our present-day pandemic, limit the resources we take for granted during normal circumstances. However, creative thinking can be bolstered in times of crisis due to the removal of resources plus the pressure of time. For example, in 1995, two physicians performed a lifesaving procedure using only the tools they had available to them in midflight. When a passenger’s lung collapsed during a 14-hour flight, the physicians used a coat hanger, a culinary knife and fork, a water bottle, and tape to perform a procedure, which saved the woman’s life.2
BUILDING A CULTURE THAT FOSTERS INNOVATION
A strong organizational culture is crucial. If leaders truly expect their teams to be innovative, they must cultivate an environment optimized for collaboration and mindful risk taking. Steven Johnson, best-selling author of Where Good Ideas Come From, researched commonalities that led to the greatest innovations in history and found seven key patterns. One of those patterns was networks where ideas could connect. He found that groundbreaking ideas did not occur in a vacuum but rather in environments conducive for sharing ideas.3
A study conducted in leading research labs showed that scientists rarely had a eureka moment at the microscope but rather through conversations with colleagues. These moments occurred at the weekly lab meeting where people shared their ideas, mistakes, and findings.4 Johnson described these types of collaborative environments as the “liquid network.”3
Health care organizations with siloed teams and departments face communication and collaboration barriers, and ultimately, improvement and innovation opportunities are stifled. The need to physically distance and go virtual due to the pandemic has exacerbated communication issues for many health care teams, although others have actually flourished, resulting in creative, innovative thinking and solutions. For the latter, the disruption to the status quo resulted in the breakdown of rigid work routines and organizational silos to an all-hands-on-deck model where multidisciplinary teams were formed, allowing new collaborations and crosspollination of ideas. As leaders, it is imperative to foster environments conducive to sharing ideas; your teams often hold the solutions you need.
In the hospital environment, multidisciplinary rounds, break rooms, conferences, lunch and learn events, and coffee shops are common places where people converse. Improved morale and camaraderie result when people are allowed to connect, sharing ideas and stories. Nurturing these opportunities becomes even more crucial because burnout among health care workers is considered the “second pandemic.” Even virtual communication can be leveraged to improve connection. Mindful and deliberate scheduling of “coffee chats,” team check-ins, retreats, adoption of collaboration platforms, and other virtual modalities can recreate prepandemic collaboration or even improve upon it. This is by no means advising to schedule meetings for the sake of having meetings but rather as leaders to recognize where your teams are naturally gravitating toward collaboration, whether physical or virtual, and foster those environments. Maintain a personalized approach using virtual conferencing technology and encourage your teams to have their cameras on because a significant amount of communication occurs through nonverbal communication. Take notice when your team members are energized by an interaction as opposed to feeling drained from it, and seek ways to support those types of networks.
THINKING DIFFERENTLY TO CREATE INNOVATIVE SOLUTIONS
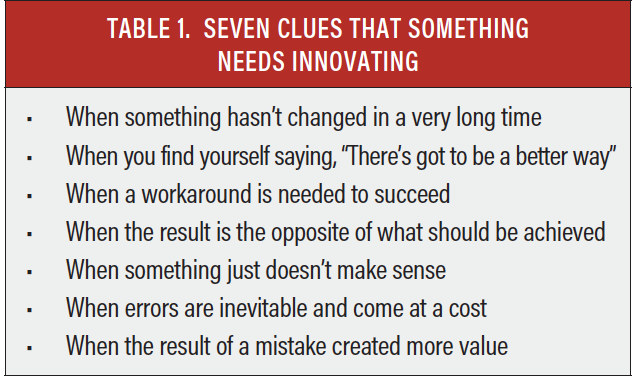
Everyone is capable of thinking differently and creatively, and everyone has the capacity to be innovative. But where do you begin to innovate? Consider the situations in Table 1. These scenarios often indicate a ripe opportunity for innovation.
Keep in mind that great ideas are often initially met with criticism and skepticism. Generally, people find it easier to be critics than creative thinkers. In fact, creative and innovative ideas often spur laughter as an initial reaction to hearing the idea. Innovators must be strong of heart—don’t be surprised when new ideas are initially met with opposition. Remember, if your idea is met with opposition, you might be on to something.
CONCLUSION
Patients rely on health care to improve health and well-being and save lives. Tragically, the COVID-19 pandemic has exacerbated the weaknesses of a reactive care delivery model that relies on a fee-for-service financial backbone. Limitations to ambulatory care and elective procedures, scarcity in resources, shortages of staff, unstable economics, and a burned-out workforce have made navigating day-to-day operations overwhelming for many organizations. When the focus is “surviving the storm,” it may feel that these extreme conditions leave no time to focus on innovation and care transformation.
Nonetheless, throughout history, the most creative, innovative solutions often arose during a crisis and emerged out of necessity. The pandemic is a Goliath of a disruptor, yet it can serve as a catalyst for change. There is a choice to either be reactive or to proactively author the future. Because the former hasn’t worked, there is no time like the present for innovation and care transformation. As the award-winning American computer scientist Alan Kay once said, “The best way to predict the future is to invent it.”5
Innovation is fundamentally optimistic because it operates with the belief that there is always a better way. MedAxiom and the American College of Cardiology share a mission: to transform cardiovascular care and improve heart health. Our purpose is to support the incredible efforts of the cardiovascular community and shape the future of cardiovascular care, together. Care transformation cannot be accomplished without innovation, and innovation cannot happen without connecting a constellation of ideas and thinking differently.
Learn more at MedAxiom.com/caretransformation.
1. Barton M, Grüntzig J, Husmann M, Rösch J. Balloon angioplasty - the legacy of Andreas Grüntzig, M.D. (1939-1985). Front Cardiovasc Med. 2014;1:15. doi:10.3389/fcvm.2014.00015
2. Associated Press. British doctor receives prize for surgery aboard airplane. Published December 7, 1995. Accessed February 8, 2022. https://apnews.com/article/a267a337b55a4fadfa9f5190b3ff62d9
3. Johnson S. Where Good Ideas Come From: The Natural History of Innovation. Riverhead Books; 2011.
4. Dunbar K. How scientists build models: invivo science as a window on the scientific mind. In: Magnani L, Neressian NJ, Thagard P, eds. Model-Based Reasoning in Scientific Discovery. Plenum Press; 1999:89-98.
5. Kay A. The best way to predict the future is to create it. But is it already too late? Presented at: Lindberg-King Lecture; September 26, 2018; Bethesda, Maryland.
Advertisement
Advertisement