Abstract
Objective
Conus region lumbosacral lipomas (LSLs) are highly heterogeneous in their morphology, clinical presentation, and outcome, with an incompletely understood natural history and often treacherous surgical anatomy. This systematic review aims to critically evaluate and assess the strength of the current LSL evidence base to guide management strategies.
Methods
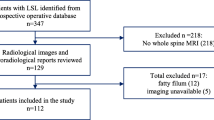
According to a systematic review following PRISMA guidelines, a search was conducted using the key term “lumbosacral lipoma” across MEDLINE (OVID), Embase, Cochrane Library, and PubMed databases from January 1951 to April 2021. All studies containing ten or more paediatric conus lipomas were included. Data heterogeneity and bias were assessed.
Results
A total of 13 studies were included, containing 913 LSLs (predominantly transitional type—58.5%). Two-thirds (67.5%) of all patients (treated and non-treated) remained clinically stable and 17.6% deteriorated. Neuropathic bladder was present in 8.6% at final follow-up. Of patients managed surgically, near-total resection vs. subtotal resection deterioration-free survival rates were 77.2–98.4% and 10–67% respectively. 4.5% (0.0–27.3%) required re-do untethering surgery. Outcomes varied according to lipoma type. Most publications contained heterogeneous populations and used variable terminology. There was a lack of consistency in reported outcomes.
Conclusion
Amongst published series, there is wide variability in patient factors such as lipoma type, patient age, and methods of (particularly urological) assessment. Currently, there is insufficient evidence base upon which to make clear recommendations for the management of children with LSL. There is an imperative for neurosurgeons, neuroradiologists, and urologists to collaborate to better standardise the terminology, assessment tools, and surgical interventions for this challenging group of conditions.






Similar content being viewed by others
References
Finn MA, Walker ML (2007) Spinal lipomas: clinical spectrum, embryology, and treatment. Neurosurg Focus 23:E10
Wykes V, Desai D, Thompson DNP (2012) Asymptomatic lumbosacral lipomas–a natural history study. Childs Nerv Syst 28:1731–1739
Sarris CE, Tomei KL, Carmel PW, Gandhi CD (2012) Lipomyelomeningocele: pathology, treatment, and outcomes. Neurosurg Focus 33:E3
Talamonti G, D’Aliberti G, Nichelatti M, Debernardi A, Picano M, Redaelli T (2014) Asymptomatic lipomas of the medullary conus: surgical treatment versus conservative management: clinical article. J Neurosurg Pediatr 14:245–254
Tu A, Hengel R, Cochrane DD (2016) The natural history and management of patients with congenital deficits associated with lumbosacral lipomas. Childs Nerv Syst 32:667–673
Patel SK, Staarmann B, Heilman A, Mains A, Woodward J, Bierbrauer KS (2019) Growing up with spina bifida: bridging the gaps in the transition of care from childhood to adulthood. Neurosurg Focus 47:E16
Chapman PH (1982) Congenital intraspinal lipomas. Pediatr Neurosurg 9:37–47
Arai H, Sato K, Okuda O, Miyajima M, Hishii M, Nakanishi H et al (1998) Diagnosis and treatment of lumbosacral lipomas. Japanese J Neurosurg pp 484–490. https://doi.org/10.7887/jcns.7.484
Arai H, Sato K, Okuda O, Miyajima M, Hishii M, Nakanishi H et al (2001) Surgical experience of 120 patients with lumbosacral lipomas. Acta Neurochir 143:857–864
Pang D, Zovickian J, Oviedo A (2009) Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode. Neurosurgery 65:511–529. https://doi.org/10.1227/01.neu.0000350879.02128.80
Morota N, Ihara S, Ogiwara H (2017) New classification of spinal lipomas based on embryonic stage. J Neurosurg Pediatr 19:428–439
Pang D, Zovickian J, Wong S-T, Hou YJ, Moes GS (2013) Surgical treatment of complex spinal cord lipomas. Childs Nerv Syst 29:1485–1513
Kanev PM, Lemire RJ, Loeser JD, Berger MS (1990) Management and long-term follow-up review of children with lipomyelomeningocele, 1952–1987. J Neurosurg 73:48–52
Cochrane DD, Finley C, Kestle J, Steinbok P (2000) The patterns of late deterioration in patients with transitional lipomyelomeningocele. Eur J Pediatr Surg 10(Suppl 1):13–17
Muthukumar N (2009) Congenital spinal lipomatous malformations: part I - Classification. Acta Neurochir 151:179–88; discussion 197
Pang D, Zovickian J, Oviedo A (2010) Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode, Part II: outcome analysis and preoperative profiling. Neurosurgery 66:253–273. https://doi.org/10.1227/01.neu.0000363598.81101.7b
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12:1495–1499
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ et al (2014) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg 12:1500–1524
National Heart, Lung, and Blood Institute (2014) Quality assessment tool for observational cohort and cross-sectional studies. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
Kulkarni AV, Pierre-Kahn A, Zerah M (2004) Conservative management of asymptomatic spinal lipomas of the conus. Neurosurgery 54:868–73; discussion 873–5
da Rosa SP, Scavarda D, Choux M (2016) Results of the prophylactic surgery of lumbosacral lipomas 20 years of experience in the Paediatric Neurosurgery Department La Timone Enfants Hospital, Marseille. France Childs Nerv Syst 32:2205–2209
Yerkes EB, Halline C, Yoshiba G, Meyer TA, Rosoklija I, Bowman R et al (2017) Lipomyelomeningocele for the urologist: should we view it the same as myelomeningocele? J Pediatr Urol 13(371):e1-371.e8
Chong S, Lee JY, Kim KH, Shin H-I, Kim K, Park K et al (2019) Radical excision of lumbosacral lipoma: an early experience of “followers.” Childs Nerv Syst 35:1591–1597
Hayashi C, Kumano Y, Hirokawa D, Sato H, Yamazaki Y (2020) Long-term urological outcomes of spinal lipoma after prophylactic untethering in infancy: real-world outcomes by lipoma anatomy. Spinal Cord 58:490–495
Valentini LG, Babini M, Cordella R, Beretta E, Destro F, Murabito P et al (2021) Early de-tethering: analysis of urological and clinical consequences in a series of 40 children. Childs Nerv Syst 37:941–949
Thompson DNP, Spoor J, Schotman M, Maestri S, Craven CL, Desai D (2021) Does conus morphology have implications for outcome in lumbosacral lipoma? Childs Nerv Syst 37:2025–2031
Fuentes M, Magalhães J, Barroso U Jr (2019) Diagnosis and management of bladder dysfunction in neurologically normal children. Front Pediatr 7:298
Sarkar S, Vora TK, Rajshekhar V (2022) Risk factors for pre-operative functional deterioration in children with lipomyelomeningocele. Childs Nerv Syst 38:587–595
Jones V, Wykes V, Cohen N, Thompson D, Jacques TS (2018) The pathology of lumbosacral lipomas: macroscopic and microscopic disparity have implications for embryogenesis and mode of clinical deterioration. Histopathology 72:1136–1144
Shane Tubbs R, Naftel RP, Rice WC, Liechty P, Conklin M, Jerry OW (2006) The patient with symptoms following resection of a lipomyelomeningocele: do increases in the lumbosacral angle indicate a tethered spinal cord? J Neurosurg Pediatr 105:62–64
Halevi PD, Udayakumaran S, Ben-Sira L, Constantini S (2011) The value of postoperative MR in tethered cord: a review of 140 cases. Childs Nerv Syst 27:2159–2162
De Vloo P, Sharma J, Alderson L, Jankovic I, Tahir MZ, Desai D et al (2022) Radical resection of lumbosacral lipomas in children: the Great Ormond Street Hospital experience. Childs Nerv Syst 38:1113–1123
Xiong Y, Yang L, Zhen W, Fangyong D, Feng W, Ting L (2018) Conservative and surgical treatment of pediatric asymptomatic lumbosacral lipoma: a meta-analysis. Neurosurg Rev 41:737–743
Author information
Ethics declarations
Conflict of interest
The authors report no disclosures and no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Perera, D., Craven, C.L. & Thompson, D. Lumbosacral lipoma in childhood, how strong is the evidence base? A systematic review. Childs Nerv Syst 40, 715–728 (2024). https://doi.org/10.1007/s00381-023-06203-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06203-9