Abstract
Objective
The objectives of the present study are the following: (a) to investigate limitations (bone height, proximity to nasopalatine nerve and roots) in juvenile patients, (b) to review the recommended site for surgical insertion (level of the maxillary first premolars), and (c) to reassess the rationale behind the manufacturer’s age limitation (12 years).
Patients and methods
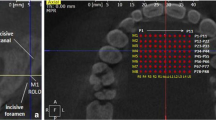
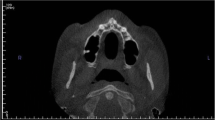
Cone beam CT images of 100 patients aged 10 to 20 years were analyzed. Vertical bone heights were measured in the median plane as well as 3- and 6-mm paramedian along the prospective axis of insertion, at the level of the first premolars (level 0), 3 mm anterior (level 1) and 3 mm posterior (level 2). The Mann-Whitney U test was used to compare bone heights between gender groups.
Results
The risk of damage to the nasopalatine nerve is highest in the median region on level 1 (46 %). The risk was lowest in the midsagittal region on level 0 (recommended insertion site; 3 %) and level 2 (0 %), as well as paramedian on levels 0 and 2. The risk of damaging roots was irrelevant for median insertion at all levels; the only critical region was 6-mm paramedian on level 1.
Conclusions
The recommendation of surgical insertion at the level of the maxillary first premolars is still justified, but a slightly more posterior implant position might improve safety. We found no relevant growth-related changes in the vertical bone heights in the median palatal area. Thus, our data do not support the strict 12-year age restriction for palatal implants.




Similar content being viewed by others
References
Bornstein MM, Balsinger R, Sendi P, von Arx T (2011) Morphology of the nasopalatine canal and dental implant surgery: a radiographic analysis of 100 consecutive patients using limited cone-beam computed tomography. Clin Oral Implants Res 22:295–301
Camargo IB, van Sickels JE (2015) Surgical complications after implant placement. Dent Clin N Am 59:57–72
Liang X, Jacobs R, Martens W, Hu Y, Adriaensens P, Quirynen M, Lambrichts I (2009) Macro- and micro-anatomical histological and computed tomography scan characterization of the nasopalatine canal. J Clin Periodontol 36:598–603
De Oliveira-Santos C, Rubira-Bullen IR, Monteiro SA, Leon JE, Jacobs R (2013) Neurovascular anatomical variations in the anterior palate observed on CBCT images. Clin Oral Implants Res 24:1044–1048
López Jornet P, Boix P, Sanchez Perez A, Boracchia A (2014) Morphological characterization of the anterior palatine region using cone beam computed tomography. Clin Implant Dent Relat Res. doi:10.1111/cid.12271
Thakur AR, Burde K, Guttal K, Naikmasur VG (2013) Anatomy and morphology of the nasopalatine canal using cone-beam computed tomography. Imaging Sci Dent 43:273–281
Artzi Z, Nemcovsky CE, Bitlitum I, Segal P (2000) Displacement of the incisive foramen in conjunction with implant placement in the anterior maxilla without jeopardizing vitality of nasopalatine nerve and vessels: a novel surgical approach. Clin Oral Implants Res 11:505–510
Katsoulis J, Enkling N, Takeichi T, Urban IA, Mericske-Stern R, Avrampou M (2012) Relative bone width of the edentulous maxillary ridge. Clinical implications of digital assessment in presurgical implant planning. Clin Implant Dent Relat Res 14(Supplement 1):e213–e223
Jacob S, Zelano B, Gungor A, Abbott D, Naclerio R, McClintock MK (2000) Location and gross morphology of the nasopalatine duct in human adults. Arch Otolaryngol Head Neck Surg 126:741–748
Peñarrocha M, Carrillo C, Uribe R, Garcia B (2009) The nasopalatine canal as an anatomic buttress for implant placement in the severely atrophic maxilla: a pilot study. Int J Oral Maxillofac Implants 24:936–942
Peñarrocha D, Candel E, Guirado JL, Canullo L, Peñarrocha M (2014) Implants placed in the nasopalatine canal to rehabilitate severely atrophic maxillae: a retrospective study with long follow-up. J Oral Implantol 40:699–706
Fäh R, Schätzle (2014) Complications and adverse patient reactions associated with the surgical insertion and removal of palatal implants: a retrospective study. Clin Oral Implants Res 25:653–658
Jung BA, Wehrbein H, Heuser T, Kunkel M (2011) Vertical palatal bone dimensions on lateral cephalometry and cone-beam computed tomography: implications for palatal implant placement. Clin Oral Implants Res 22:664–668
Greenstein G, Tarnow D (2006) The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol 77:1933–1943
Ali Alhassani AA, AlGhamdi AS (2010) Inferior alveolar nerve injury in implant dentistry: diagnosis, causes, prevention, and management. J Oral Implantol 36:401–407
Vazquez L, Saulacic N, Belser U, Bernard JP (2008) Efficacy of panoramic radiographs in the preoperative planning of posterior mandibular implants: a prospective clinical study of 1527 consecutively treated patients. Clin Oral Implants Res 19:81–85
Worthington P (2004) Injury to the inferior alveolar nerve during implant placement: a formula for protection of the patient and clinician. Int J Oral Maxillofac Implants 19:731–734
Dahlberg G (1940) Statistical methods for medical and biological students. Interscience Publication, New York
Wehrbein H, Göllner P, Diedrich P (2008) Orthodontic load on short maxillary implants with reduced sink depth: an experimental study. Clin Oral Implants Res 19:1063–1068
Chang SH, Lin CL, Lin YS, Hsue SS, Huang SR (2012) Biomechanical comparison of a single short and wide implant with monocortical or bicortical engagement in the atrophic posterior maxilla and a long implant in the augmented sinus. Int J Oral Maxillofac Implants 27:e102–e111
Rettinger G, Engelbrecht-Schnür S (1995) Palatal sensory impairment after septoplasty. Lanryngorhinootologie 74:282–285
Chandra RK, Rohman GT, Walsh WE (2008) Anterior palate sensory impairment after septal surgery. Am J Rhinol 22:86–88
Asscherickx K, Hanssens JL, Wehrbein H, Sabzevar MM (2005) Orthodontic anchorage implants inserted in the median palatal suture and normal transverse maxillary growth in growing dogs: a biometric and radiographic study. Angle Orthod 75:826–831
Jung BA, Kunkel M, Göllner P, Liechti T, Wagner W, Wehrbein H (2012) ) Prognostic parameters contributing to palatal implant failures—a long-term survival analysis of 239 patients. Clin Oral Implants Res 23:746–750
Acknowledgments
We thank Kerstin Vach from the Institute of Biometry, University of Freiburg, and Jessica Hirsch from the Institute of Biometry, University of Witten/Herdecke, for statistical advice and support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The present study was funded by the authors’ own institution.
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
The retrospective study was approved by the institutional review board of Ruhr University, Bochum, Germany [no.: 4093-11].
Informed consent
For this type of study, formal consent is not required.
Additional information
Martin Kunkel and Britta A. Jung contributed equally and, therefore, share senior authorship.
Rights and permissions
About this article
Cite this article
Kawa, D., Kunkel, M., Heuser, L. et al. What is the best position for palatal implants? A CBCT study on bone volume in the growing maxilla. Clin Oral Invest 21, 541–549 (2017). https://doi.org/10.1007/s00784-016-1913-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1913-1