Table of Contents
What do we understand by Safe motherhood?
- Safe motherhood is the concept or initiatives to ensure that women receive high quality care in order to achieve the optimum level of health of mother and infant.
- Safe motherhood is designed in a way that the women is ensured of high-quality gynecological, family planning, prenatal, delivery and postpartum care.
- Safe motherhood aims at improving maternal and child health and eliminating the probable risk that can occur.
- Safe motherhood is required for obtaining the desired outcome of pregnancy.
- The goal of the Safe Motherhood Program is to reduce maternal and neonatal morbidity and mortality and to improve the maternal and neonatal health through preventive and promotive activities as well as by addressing avoidable factors that cause death during pregnancy, childbirth and postpartum period
- Safe pregnancy, safe delivery and safe birth of new born are the major components of safe motherhood. These components are achieved through the principles of safe motherhood.
- Safe motherhood also ensures the safety of overall pregnancy and health of mother and child
Why safe motherhood?
- In 2007 there were at least 3.2 million stillborn babies, 4 million neonatal deaths and more than half a million maternal deaths globally.
- Every day in 2015, about 830 women died due to complications of pregnancy and child birth. Most of these could have been prevented.
- Maternal and neonatal deaths are still high and unacceptable.
- Over half of maternal deaths are due to preventable or treatable conditions.
- The maternal morbidity and mortality can be reduced through preventive and promotive activities and by addressing avoidable factors that cause death, which are included in safe motherhood initiatives.
- For newborns, most deaths are due to premature birth, infections and complications of asphyxia, again all preventable or treatable conditions.
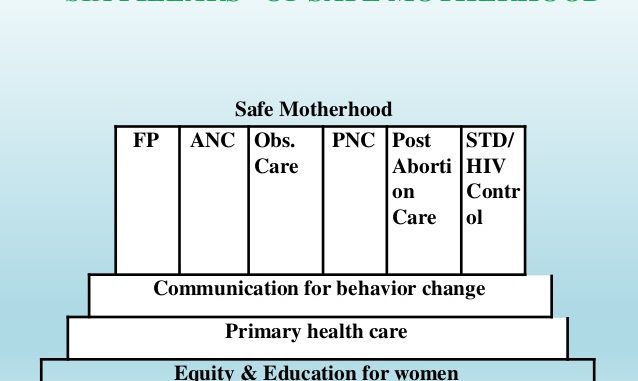
Pillars of safe motherhood:
Pillars of safe motherhood can also be considered as the principles of safe motherhood
The basic pillars/principles of safe motherhood are:

1. Family Planning:
- FP is an important component of safe motherhood
- It is necessary to ensure that individuals and couples have adequate information and services regarding FP
- FP is also necessary to plan the timing, number of children, spacing between pregnancies, delay pregnancy, etc.
2. Antenatal Care (ANC)
- ANC checkup is necessary to detect complications early and treat them as soon as possible
- It is also essential to provide pregnant women with vitamin supplements, iron tablets and vaccinations so that they can have a healthy and strong pregnancy.
3. Obstetric and Newborn Care
- Obstetric and newborn care refers to all the care and health care level initiatives provided to the mother and newborn to reduce maternal and newborn mortality and morbidity.
- Birth attendants should have the knowledge, skills, and equipment to perform a clean and safe delivery.
- Moreover, emergency care for high-risk pregnancies and complications are made available to all women and newborn who need it.
3.1 Essential Obstetric and Newborn Care (EONC):
- Essential obstetric and newborn care encompasses all care that is provided during pregnancy, labor, childbirth and postpartum period to prevent and manage complications.
- It is a term used to describe the elements of obstetric and newborn care needed for the management of normal and complicated pregnancy, delivery, postpartum period.
Essential Obstetric and Newborn Care is differentiated into two levels:
3.1.1 Basic Emergency Obstetric and Newborn Care (BEmONC)
It includes following signal functions (i.e., key interventions to treat/manage key causes of maternal and newborn mortality):
 Management of pregnancy complications by assisted vaginal delivery (using vacuum extractor or forceps)
Management of pregnancy complications by assisted vaginal delivery (using vacuum extractor or forceps)- Availability/administration of antibiotics
- Availability/administration of sedatives and anticonvulsants for eclampsia
- Availability/Administration of parenteral Uterotonics (a drug that causes contraction of uterus) like oxytocin, ergometrine, misoprostol, or prostaglandin etc. *(Note: Ergometrine should NEVER be given to a woman with elevated blood pressure because it can precipitate an eclamptic seizure/convulsion.)
- Availability/Administration of parental drugs (for PPH, infection and pre-eclampsia and eclampsia
- Manual removal of placenta
- Manual removal of retained products of conception. (facilitated with a manual vacuum aspirator or dilatation & curettage (D&C))
- Resuscitation of newborns (using a self-inflating bag and mask (Ambu bag) and room air).
- Availability/Administration of parenteral antibiotics to the newborn.
BEmONC services are usually provided at the primary health care levels by skilled birth attendants of any cadre.
3.1.2 Comprehensive Emergency Obstetric and Newborn Care (CEmONC):
It includes all the services of basic essential obstetric services along with following additional services:
- Cesarean section/surgery
- Blood transfusion
- Anesthesia
- Umbical vein insertion and
- Intubation of the newborn
CEmONC services are basically provided at the referral hospitals by physicians, clinicians or specially trained midwives.
4. Postnatal Care (PNC)
- It is necessary to ensure that postpartum care is provided to the mother and baby.
- It includes counselling mothers about child handling, exclusive breast feeding, etc.
- Moreover, PNC also comprises of providing awareness regarding the FP, and managing the danger signs and symptoms seen in both mother and child.
5. Post abortion Care
- It is necessary to prevent complications of abortion.
- Post abortion care helps to identify/detect if there are any complications of abortion.
- Useful to refer other reproductive health problems when necessary.
- An essential element of post abortion care services is providing the woman with a family planning method before she leaves the facility.
- It also provides counselling and awareness about different family planning methods.
Essential Elements of Post Abortion Care (PAC) services are:
- Emergency treatment of incomplete abortion and potentially life-threatening complications .
- Post abortion family planning counseling and services.
- Links between emergency PAC services and other reproductive health care.
6. STD/HIV/AIDS Control
- HIV screening is done to prevent, and manage HIV and AIDS transmission to the baby
- To assess risk for future infection
- To provide voluntary counseling and testing
- To expand services to address mother to child transmission.
Major factors contributing to morbidity and mortality during motherhood:
Direct cause for the majority of maternal deaths are:
1. Severe bleeding
- Mostly bleeding after childbirth
- Includes antepartum, postpartum, abortion, and ectopic pregnancy.
2. Infections
- Usually after childbirth
- Includes infection of the uterus, tubes, urinary system and fetal infection.
- Also caused due to unhygienic delivery site and practice
3. High blood pressure during pregnancy
- Includes pre-eclampsia and eclampsia
4. Complications from delivery
- Several complications can arise during the pregnancy
- Teenage pregnancy, advanced maternal age, parity, etc and many other factors can cause complications
5. Unsafe abortion
- Common cause of maternal death
- Unsafe abortions are high in countries where abortion is not legalized
These factors contribute to nearly 75% of all maternal deaths.
Indirect causes:
a) 3 delays
Three delays usually refer to:
- Delay in the decision to seek care (seeking care)
- Delay arrival at a health facility (reaching care) and
- Delay in obtaining the adequate treatment (receiving care)
These delays contribute to increase the complication in pregnancy. However, these delays are determined by the educational status, financial status, accessibility of health care and services, etc.
b) Accessibility
- Health services and facilities are still not available in every knock and corner of many countries
- Reaching health facility is often riskier in some places
- Lack of accessibility promotes the delay
c) Poverty
- Poverty is the other important factor contributing to maternal deaths
- People of rural areas do not fancy health services
- Seeking health services often is not the priority to those people who have to worry about hands to mouth
d) Cultural practices
- Traditional practices often prevent individual from seeking health care
- Cultural practices also determine the care given to pregnant women, food practices, etc.,
- Unsafe abortion is also an example of cultural practices.
References and for More Information:
http://www.policyproject.com/matrix/SafeMotherhood.cfm
http://www.who.int/bulletin/volumes/85/10/07-045963/en/
http://www.fhd.gov.np/index.php/en/2014-03-21-09-41-44/safe-motherhood
https://www.womenandchildrenfirst.org.uk/maternal-mortality
http://www.who.int/gho/maternal_health/mortality/maternal_mortality_text/en/
http://www.policyproject.com/pubs/advocacy/MaternalHealth/AM_MH_16Sec3-2.pdf
http://publichealthinnepal.blogspot.com/2016/05/essentials-of-safe-motherhood.html
http://primelactationcentercameroon.blogspot.com/2012/12/four-pillars-of-safe-motherhood_3618.html
https://eige.europa.eu/rdc/thesaurus/terms/1356
http://www.who.int/news-room/fact-sheets/detail/maternal-mortality
https://www.parashospitals.com/parasbliss/blogs/pillars-of-safe-motherhood/