One of the complications of Morton’s neuroma surgery and Morton’s neuroma corticosteroid injections is Fat Pad Atrophy. It causes significant foot pain and metatarsalgia.
The fat pad is the the thick pad of connective tissue that runs under the ball and heel of the foot and forms the lower aspect of foot. The purpose of the fat pad is:
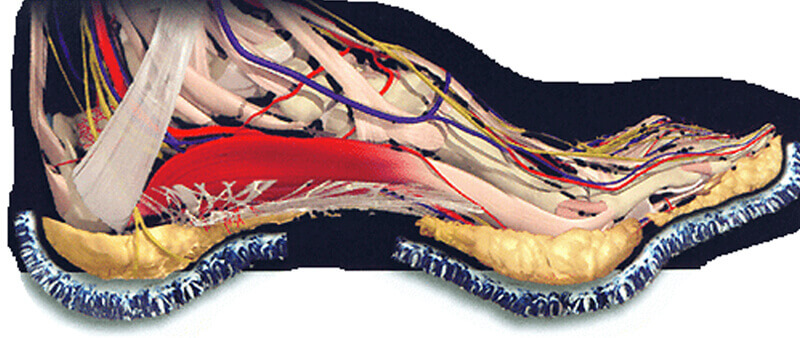
Fat pad atrophy the gradual loss of the fat pad in the ball or heel of the foot. Conditions like fat pad atrophy of the foot are more common in aging population and usually presents with severe foot pain during walking. Fat Pad atrophy is the thinning of the pad that exposes the delicate connective tissue elements to strain and pressure creating inflammation and micro-injury. In poorly managed cases, patients present with severe pain and discomfort.
Some characteristic symptoms of fat pad atrophy include:
The risk profile and prevalence of fat pad atrophy is fairly comparable in males and females. However, some experts believe that females are relatively more vulnerable to develop this condition because of:
Certain factors that may aggravate the risk of developing Fat Pad Atrophy such as:
When conventional methods fail, healthcare providers may recommend surgical treatment as a last resort.
References:
By providing us with your information you are consenting to the collection and use of your information in accordance with our Terms of Service and Privacy Policy.