Abstract
Introduction and aims
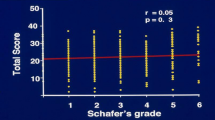
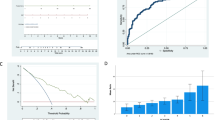
Family physicians are limited by lack of tools to monitor benign prostate hyperplasia. VAUS provides a cost-effective, easily administered non-invasive tool. Our primary aim was to validate VAUS correlation with uroflowmetry measured maximal flow rate (Qmax), voided volume and International Prostate Symptom Scores (IPSS) symptom scores. Secondary aim was to study how the VAUS fared at predicting poor flow (Qmax < 10 ml/s) compared to age, voided volume and IPSS. Tertiary aim was to predict the best VAUS as a cutoff for poor flow.
Methods
After IRB approval, 1000 patients were prospectively recruited. They had VAUS, uroflowmetry and IPSS performed. VAUS is a novel five-point visual analogue scoring of urine flow, with one being the weakest and five the strongest. Data were analysed using SPSS where spearman’s correlation coefficient and logistic regression analysis were performed looking for significance. Receiver operating curves (ROC) curves were used to identify best VAUS cutoff.
Results
1000 patients were studied with mean age of 68.99 (50–95). VAUS showed good correlation with Qmaxp < 0.001, voided volume p = 0.006 and IPSS p <0.001. On multivariate analysis both VAUS and voided volume predicted poor flow significantly with p value of<0.001 and p =0.001, respectively. On ROC analysis VAUS of 2.5 was identified as best value for predicting poor flow with p value <0.001.
Conclusion
VAUS is a validated tool for monitoring of lower urinary tract symptoms in our patients showing significant correlation with uroflowmetry, voided volume and IPSS.





Similar content being viewed by others
References
Thorpe A, Neal D (2003) Benign prostatic hyperplasia. Lancet 361(9366):1359–1367
Foo KT (2016) Solving the benign prostatic hyperplasia puzzle. Asian J Urol. 3(1):6–9
Roehrborn CG (2008) BPH progression : concept and key learning from MTOPS. ALTESS, COMBAT and ALF-ONE, BJU Int 101(suppl 3):17–21
Rodrigues Netto N Jr., de Lima ML, de Andrade EF et al (1997) Latin American study on patient acceptance of the International Prostate Symptom Score (IPSS) in the evaluation of symptomatic benign prostatic hyperplasia. Urology 49(1):46–49
Cam K, Akman Y, Cicekci B, Senel F, Erol A (2004) Mode of administration of international prostate symptom score in patients with lower urinary tract symptoms: physician vs self. Prostate Cancer Prostatic Dis 7(1):46–49
Van der Walt CLE, Heyns CF, Groeneveld AE, Edlin RS, van Vuuren SPJ (2011) Prospective comparison of a new visual prostate symptoms score versus the international prostate symptoms score in men with lower urinary tract symptoms. Urology 78(1):17–20
Foo KT, Ho SSH, Wong M, Lim KB, Teo CCP et al (2017) Singapore urological association clinical guidelines for male lower urinary tract symptoms/benign prostate hyperplasia. Singapore Med J 58(8):473–480
Graves S, Cornu JN, Gacci M, Gratzke C, Hermann TRW et al (2019) European association of urology guidelines panel non-neurogenic male lower urinary tract symptoms. Eur Urol 67(6):1099–1109
Gupta DK, Gupta S, Jha N (2015) Correlation between visual prostate symptoms score and uroflowmetry parameters in patients with benign enlargemet of prostate. J Nepalgunj Med Coll 13(2):2–5
Teillac P, Rozet F, Terrier N, Mongiat-Artus P, Rambeaud JJ (2004) Value of a visual analogue scale for evaluation of the severity of symptoms of benign prostate hyperplasia (BPH): pilot study of 2 urological centres. Prog Urol 14(4):493–500 (Discussion 499)
Bosch JL, Hop WC, Kirkels WJ, Schroder FH (1995) The international prostate symptom score in a community based sample of men between 55 and 74 years of age: prevalence and correlation of symptoms with age, prostate volume, flow rate and residual urine volume. Br J Urol 75(5):622–630
Groeneveld AE, Heyns CF, van der Walt CLE (2012) Correlation between a new visual prostate symptoms score (VPSS) and uroflowmetry parameters in men with lower urinary tract symptoms. S Afr Med J 102(4):237–240
Golomb J, Lindner A, Siegel Y, Korzak D (1992) Variability and circadian changes in home uroflowmetry in patients with benign prostate hyperplasia compared to normal controls. J Urol 147(4):1044–1047
Acknowledgements
We would like to acknowledge the support of Sing health Academic Clinical Program Innovation Grant for funding this project. In addition we acknowledge our urology clinical laboratory nurses led by Senior Staff Nurse Esther Ho for the groundwork in running the project (Grant No. 2017).
Author information
Authors and Affiliations
Contributions
RT: project development, data collection, manuscript writing. MYN: data management, data analysis. SHN: data collection, project development. RM: project development. HH: project development.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures in the studies involving human participants were in accordance with ethical standards of the institution (Singhealth IRB 2016/2746) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This project has been presented and awarded at several conferences. Best abstract presentation UAA 2017 meeting Hong Kong, Best poster SIU 2018 Seoul and Best poster at Urofair 2019 Singapore. It was also presented as a moderated poster at EAU 2019 Barcelona.
Rights and permissions
About this article
Cite this article
Tiwari, R., Ng, M.Y., Neo, S.H. et al. Prospective validation of a novel visual analogue uroflowmetry score (VAUS) in 1000 men with lower urinary tract symptoms (LUTS). World J Urol 38, 1267–1273 (2020). https://doi.org/10.1007/s00345-019-02909-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02909-1