Professional Documents
Culture Documents
Perioperative Management For A Patient With Severe Congenital Factor V Deficiency Undergoing Cochlear Implantation
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Perioperative Management For A Patient With Severe Congenital Factor V Deficiency Undergoing Cochlear Implantation
Copyright:
Available Formats
Volume 7, Issue 6, June – 2022 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Perioperative Management for a Patient with Severe
Congenital Factor V Deficiency Undergoing Cochlear
Implantation
Zineb Bahja, Hanaa Bencharef, Sofia Sraidi, Bouchra Oukkache
Hematology Laboratory, CHU Ibn Rochd, Casablanca, Morocco.
Hassan II University of Casablanca, Faculty of Medicine and Pharmacy of Casablanca, Morocco.
Abstract:- Congenital factor V deficiency (CFVD) is a There is no commercially available recombinant FV or
rare coagulation disorder, also known as para plasma-derived FV concentrate [5]. In some of these cases,
hemophilia, that was first described by Owren in 1947. pre-interventional fresh frozen plasma (FFP) infusions have
Until now, no specific protocols for the management of been proven to minimize bleeding [3,6] . In this work we
these patients have been established, owing to the variable report a case of a severe congenital factor V deficiency that
spectrum of bleeding manifestations. However, available was operated for cochlear implantation with FFP
research suggests that perioperative infusion of fresh infusions and no abnormal bleeding events.
frozen plasma (FFP) may aid in maintaining FV levels to
prevent bleeding. We present the case of a 47-year-old II. CASE PRESENTATION
woman with congenital FV deficiency who underwent
cochlear implantation with no postoperative hemorrhagic A 47-years-old woman candidate for a cochlear implant
complications. for which the preoperative coagulation tests showed a
significantly prolonged prothrombin time (PT) 16%
Keywords:- Factor V, Congenital Factor V Deficiency, (Reference range RR 70-140%) and an elevated activated
Perioperative Management, Cochlear Implantation, partial thromboplastin time (aPTT) 83.9s (RR 23-33s) with a
Hemostasis, Hematology, Case Report. normal level of fibrinogen 3.06g/l (RR 2-4g/l). The patient
has no history of hemorrhagic syndrome. Subsequent factors
I. INTRODUCTION assays revealed a decreased factor V activity at 1% (RR 70-
140%), the results of other factor assays was (all RR 70-
Congenital FV deficiency is identified as a rare bleeding 140%): factor II at 88%, factor X at 86% and factor VIII at
disorder (RBD), is expressed in an autosomal recessive 140% (searching for a combined factor V and VIII
manner of inheritance with an estimated incidence of one per deficiency). FV inhibitor using a mixing test (mixture of
million in the general population. The disease is mostly equal volume of patient’s plasma with normal plasma) was
prevalent in regions where parental consanguinity is normal. The family investigation revealed the existence of a
commonly practiced. The disorder can occur up to 10 times brother with isolated factor V deficiency (factor V at 1%),
more frequently [1]. FV deficiency, formerly known as concluding to a severe congenital factor V deficiency.
parahemophilia or Owren’s disease, was first described by
Paul Owren in 1943 [1,2]. Only 200 patients with factor V We established a transfusion protocol including the
deficiency have been described in the literature, and most of infusion of FFP at 20 mL/kg to control bleeding. Our
them became symptomatic in early childhood. Typical objective was to have a factor V rate > 20% with an infusion
clinical signs are mucosal tract bleeding and excessive of 5 units of FFP on day 1 preoperatively; an infusion of 5
bleeding after invasive procedures [3]. Based on the FV units of FFP on day 0; an infusion of 5 units of FFP on day 1
activity, the disease can be classified into three groups: mild postoperatively; and an infusion of 5 units of FFP on day 2.
(with FV level at 10%), moderate (with FV level < 10%), and
severe (with undetectable FV level) [4]. There are currently Coagulation assays were performed pre and post
no well-established protocols for managing these patients. infusion of FFP (Figure 1).
IJISRT22JUN771 www.ijisrt.com 793
Volume 7, Issue 6, June – 2022 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Fig 1: The value of clinical blood coagulation analysis for the patient before and after surgery.
70% 100
93.2 64% 90
60% 56%
54%
55% 80
50% 70
60
40%
FV and PT (%)
35%
50
30% 36.5 aPTT
23% 40
(s)
31.4
20% 30
15% 30.6
19% 31.2 20
17%
10%
10
1%
0% 0
D-2 D-1 D0 D1 D2
PT (%) 15% 56% 64% 54% 55%
Factor V (%) 1% 19% 35% 23% 17%
aPTT (s) 93.2 36.5 30.6 31.2 31.4
The level of factor V increased by 35% compared to It is a glycoprotein generated by the liver, with around
normal during the infusion of FFP. The levels of aPTT and 80% of it found in plasma and 20% in platelet alpha granules
PT were corrected to 70% of normal after the infusion of the [10,5]. FV is a procoagulant cofactor that helps to create
FFP. fibrin by causing prothrombin to develop. Thrombin, which
is created through a different activation mechanism, catalyzes
During and after the surgery, no evidence of active FV activation. Factor Va (FVa) activates factor Xa (FXa) in
bleeding or major complications were reported, and the the second phase of the coagulation cascade, leading to the
patient was discharged after 3 days. During the one month conversion of prothrombin to thrombin. FV interferes with
follow-up, she had no evidence of bleeding. the anticoagulant cascade by inhibiting factor VIII activity
[11].
III. DISCUSSION
The clinical features and family history, as well as
Congenital Factor V deficiency is thought to be passed routine and specific laboratory tests, are used to make the
down through families via an autosomal recessive gene (q23- diagnosis of FV deficiency. Concurrent prothrombin time
24)2, which affects one in every million people and has no (PT) and activated partial thromboplastin time (aPTT)
gender or race association [7]. Clinical symptoms of FV prolongation is required before performing more specific
deficiency vary in severity and type. They vary in severity assays, such as the FV activity assay. In the case of low FV
from minor mucosal and soft tissue bleeding to potentially activity, mixing studies should be performed to rule out the
fatal hemorrhage such as gastrointestinal and cerebral presence of an FV inhibitor. To rule out the possibility of
bleeding [6]. The most common manifestations in later life combined FV and FVIII deficiency, the FVIII level must also
are mucous hemorrhages, most commonly epistaxis in men be determined. Molecular analysis can also be used to
and menorrhagia in women [8]. confirm the disease [12].
The vast majority of FV deficiency-causing mutations Despite the fact that our patient had no history of
are one-of-a-kind and limited to a single family or region [4]. significant bleeding, preoperative laboratory testing revealed
One-third of all hereditary genetic disorders are caused by a prolonged PT and aPTT as well as an FV level of 1%. A
premature termination codon mutations (PTC). PTC is a type family investigation revealed the existence of a brother with
of nonsense-mediated mRNA decay (NMD) that contains isolated factor V deficiencyAccording to some researchers,
translation [9]. PTC-causing mutations have long been linked residual platelet FV may be critical for maintaining proper
to severe forms of FV deficiency [4]. hemostasis in people with FV levels below 1%, which could
IJISRT22JUN771 www.ijisrt.com 794
Volume 7, Issue 6, June – 2022 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
explain the difference between FV levels and different [5]. Thakar K, Parikh K, Chen Y, et al. Isolated factor V
bleeding presentations [10]. deficiency in a patient with elevated PT and a PTT
during routine pre-operative laboratory screening. Stem
Because of its rarity, no guidelines or protocols for Cell Investig. 2014;1:1–4.
treating this unusual entity have been developed [6]. When a [6]. Alexa Bello,Eric Salazar, Kirk Heyne, and Joseph
factor V concentrate was unavailable, FFP was the best factor Varon. Aortic Valve Replacement in Severe Factor V
substitute. To reduce the bleeding, we infused FFP at a rate Deficiency and Inhibitor: Diagnostic and Management
of 20 mL/kg before and after surgery to raise FV levels. In Challenges. Cureus. 2019 Oct; 11(10): e5918.
cases of invasive testing, bleeding, or surgery, FFP maintains [7]. Peyvandi F, Mannuci PM. Rare coagulation disorders.
FV activity at >25 percent to 30 percent [5,13,14], which is Thromb Heamost 1999;84:1207-14.
similar to our case. [8]. Lak M, Sharifian R, Peyvandi F, Mannucci PM.
Symptoms of inherited factor V deficiency in 35 Iranian
With no signs of severe bleeding, our patient received patients. Br J Haematol 1998;103:067-69.
five units of FFP on Day -1, Day 0 (3H preoperatively), and [9]. Frischmeyer PA, Dietz HC. Nonsense-mediated mRNA
Day 1 postoperatively, and was discharged three days later decay in health and disease. Hum Mol Genet.
with no current bleeding or major problems. Some authors 1999;8(10):1893–1900.
recommended FFP transfusions three to ten days after surgery [10]. Park YH, Lim JH, Yi HG, et al. Factor V deficiency in
to maintain FV levels and prevent hemorrhage [15]. Korean patients: clinical and laboratory features,
treatment, and outcome. J Korean Med Sci.
IV. CONCLUSION 2016;31:208–213.
[11]. Camire RM. A new look at blood coagulation factor
In patients with prolonged PT and aPTT, congenital FV V.Curr Opin Hematol. 2011;18:338–342.
deficiency should be explored. Major surgical treatments can [12]. Tabibian S, Kazemi A, Dorgalaleh A. Laboratory
be carried out on those people. Assuming that FV levels are diagnosis of congenital factor V deficiency, routine,
carefully monitored prior to surgery, the precise role and specific coagulation tests with molecular methods. J
application of FFP in these challenging situations remains to Cell Mol Anesth. 2016;1(02):87–90.
be defined. [13]. Mannucci PM, Duga S, Peyvandi F. Recessively
inherited coagulation disorders. Blood. 2004;104:1243–
Competing interests 52.
There are no competing interests declared by the [14]. Giancarlo Castaman. Prophylaxis of bleeding episodes
authors. and surgical interventions in patients with rare inherited
coagulation disorders.Blood Transfus. 2008 Sep;
Authors’ contributions 6(Suppl 2): s39–s44.
The diagnosis and clinical management of the patient [15]. Husain S, Ballem N, Beaton HL. Gastric bypass in a
were the responsibility of ZB, BO, and SS. The paper was factor V deficient patient. Obes Surg. 2006;16:1104–
written by ZB. HB assisted with the initial draft's analysis, 1106.
supervision, and writing. BO conducts an intellectual content
evaluation and edits the paper. The final manuscript was read
by all authors and approved by them.
REFERENCES
[1]. Tabibian S, Shiravand Y, Shams M. A Comprehensive
Overview of Coagulation Factor V and Congenital
Factor V Deficiency. Semin Thromb Hemost.
2019;45:523–543.
[2]. Lippi G, Favaloro EJ, Montagnana M, Manzato F, Guidi
GC, and Franchini M. Inherited and acquired factor V
deficiency. Blood Coagul Fibrinolysis.
2011;22(03):160–166.
[3]. Meidert AS, Kinzinger J, Möhnle P. Perioperative
Management of a Patient with Severe Factor V
Deficiency Presenting with Chronic Subdural
Hematoma: A Clinical Report. World Neurosurg. 2019
Jul;127:409-413.
[4]. Thalji N, Camire RM. Parahemophilia: new insights
into factor v deficiency. Semin Thromb Hemost.
2013;39(06):607–612.
IJISRT22JUN771 www.ijisrt.com 795
You might also like
- Face Mask WaiverDocument2 pagesFace Mask WaiverLive 5 News0% (1)
- CHCFAM003 Student Assessment Task 1Document19 pagesCHCFAM003 Student Assessment Task 1kishor khatriNo ratings yet
- Sexual and Gender IdentityDocument28 pagesSexual and Gender IdentityCaroline AlagadmoNo ratings yet
- Case Write Up 2Document4 pagesCase Write Up 2E learningNo ratings yet
- Blood Circulation System 10 PDFDocument29 pagesBlood Circulation System 10 PDFSardar jiNo ratings yet
- Circulating Tumor Cells (Dr. Minetta Liu)Document34 pagesCirculating Tumor Cells (Dr. Minetta Liu)National Press FoundationNo ratings yet
- Fy20 + Fy21Td Med Path Data: Casey McgrathDocument4 pagesFy20 + Fy21Td Med Path Data: Casey McgrathChadNo ratings yet
- HCC - Improve CareDocument37 pagesHCC - Improve Caregiorgi popiashviliNo ratings yet
- Metastasisandlocalinvasionpatternofbladderca PDFDocument8 pagesMetastasisandlocalinvasionpatternofbladderca PDFAkhmad MustafaNo ratings yet
- 03_ SÀNG LOC QUÝ 2 ( Tiếng Anh )Document48 pages03_ SÀNG LOC QUÝ 2 ( Tiếng Anh )huyentruonghmNo ratings yet
- Semen Analysis: Syed Mahsan HussainDocument1 pageSemen Analysis: Syed Mahsan Hussainmedicine ki dunia OfficialNo ratings yet
- Prof. Lesmana - The 4th Liv GI Fair PGC On Hepatitis C Evolution of DAA (Direct Acting Antiviral AgentDocument26 pagesProf. Lesmana - The 4th Liv GI Fair PGC On Hepatitis C Evolution of DAA (Direct Acting Antiviral AgentWenny NgawingNo ratings yet
- Study of Clinical Profile, Risk-Factors and Management of Post Partum Haemorrhage in A Tertiary Care CentreDocument5 pagesStudy of Clinical Profile, Risk-Factors and Management of Post Partum Haemorrhage in A Tertiary Care CentreIJAR JOURNALNo ratings yet
- Kevin J. Bozic, MD, MBA: Harry E. Rubash, MDDocument48 pagesKevin J. Bozic, MD, MBA: Harry E. Rubash, MDHervis FantiniNo ratings yet
- Peripartum Hysterectomy - Incidence, Indications, Risk Factors and Outcomes at A Teritiary Care HospitalDocument4 pagesPeripartum Hysterectomy - Incidence, Indications, Risk Factors and Outcomes at A Teritiary Care HospitalIJAR JOURNALNo ratings yet
- Anaemia in Transplant Patients Ppt2034Document36 pagesAnaemia in Transplant Patients Ppt2034josemylackalNo ratings yet
- Paparan Capaian TB RO Tahun 2022 (Data Update 19 Okt 2022)Document16 pagesPaparan Capaian TB RO Tahun 2022 (Data Update 19 Okt 2022)Titi YulianaNo ratings yet
- Surgical Treatment of Secondary Peritonitis: A Continuing ProblemDocument6 pagesSurgical Treatment of Secondary Peritonitis: A Continuing ProblemAstutikNo ratings yet
- ASSIGNMENTDocument12 pagesASSIGNMENTArthur FrancisNo ratings yet
- ANANT KUMAR - TenecteplaseDocument37 pagesANANT KUMAR - Tenecteplaseanantsrivastava85No ratings yet
- Managing Colorectal Liver MetastasesDocument66 pagesManaging Colorectal Liver MetastasesFlaviusNo ratings yet
- Akses Hemodialisis Yang Optimal Berdasarkan Perspektif Nefrologis (Webinar B.TKV 5 Sept 2020) (Edited)Document39 pagesAkses Hemodialisis Yang Optimal Berdasarkan Perspektif Nefrologis (Webinar B.TKV 5 Sept 2020) (Edited)puji kristiniNo ratings yet
- Primary Endpoint: Hospital Survival Following Implantation of ECMO in Adult Cardiac Surgery Patients With Refractory Cardiotomy CardiogenicDocument1 pagePrimary Endpoint: Hospital Survival Following Implantation of ECMO in Adult Cardiac Surgery Patients With Refractory Cardiotomy CardiogenicPriya Nair MenonNo ratings yet
- Prevalence of Surgical Site Infection in Orthopaedic SURGERY: A 3year AnalysisDocument18 pagesPrevalence of Surgical Site Infection in Orthopaedic SURGERY: A 3year AnalysissidcurieNo ratings yet
- A Delphi Consensus-Based Chronic Pelvic Pain Standardized Ultrasound ApproachDocument14 pagesA Delphi Consensus-Based Chronic Pelvic Pain Standardized Ultrasound ApproachSharon Cristine Paroneto de SousaNo ratings yet
- 4 MOUREY Actualités Cancer Du Rein Onco Occitanie 12 Janvier 2023Document41 pages4 MOUREY Actualités Cancer Du Rein Onco Occitanie 12 Janvier 2023Mihary RamanandraitsioryNo ratings yet
- 1.3.3 Diarrhea-4 Januari-3 JanDocument56 pages1.3.3 Diarrhea-4 Januari-3 JanmaryamNo ratings yet
- CQI HIM August 2021 PRHDocument16 pagesCQI HIM August 2021 PRHAbdur Rashid KhanNo ratings yet
- Simple Population of The Study 1458Document20 pagesSimple Population of The Study 1458Abdirahman Hassan MohamedNo ratings yet
- Geetha KDocument6 pagesGeetha Kdkhatri01No ratings yet
- CD PRM 6 MonthsDocument33 pagesCD PRM 6 MonthsderejrNo ratings yet
- Dr. Arya Govinda - Management of OAB in ElderlyDocument36 pagesDr. Arya Govinda - Management of OAB in ElderlyCOVID RSHJNo ratings yet
- Hassen Y ReportDocument5 pagesHassen Y ReportXasan YusufNo ratings yet
- Geita Gold Mine MD Safety MeetingDocument50 pagesGeita Gold Mine MD Safety MeetingStephen MadahaNo ratings yet
- Hasil Analisis Survei Budaya PasienDocument47 pagesHasil Analisis Survei Budaya Pasienanon_711785155No ratings yet
- Palm Fisting, Thrombophlebitis, IV Cannulated Patient, VIP Score (Visual Infusion Phlebitis)Document8 pagesPalm Fisting, Thrombophlebitis, IV Cannulated Patient, VIP Score (Visual Infusion Phlebitis)Manashi SenguptaNo ratings yet
- Sample Size Calculation for Subdural Hematoma StudyDocument53 pagesSample Size Calculation for Subdural Hematoma StudyAkhileshNo ratings yet
- Sample Size CalculationDocument52 pagesSample Size CalculationAkhileshNo ratings yet
- Examination Performance Report Spring 2018 Part 1Document3 pagesExamination Performance Report Spring 2018 Part 1Syed Danish AliNo ratings yet
- VTE ProphylaxisDocument17 pagesVTE ProphylaxisPeter McManusNo ratings yet
- Challenges in Hypertension ManagementDocument86 pagesChallenges in Hypertension ManagementAdel SALLAMNo ratings yet
- Hepatitis BDocument13 pagesHepatitis BFemi luwitaNo ratings yet
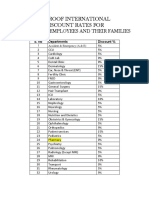
- Discount Summary of PTADocument1 pageDiscount Summary of PTAAnwarNo ratings yet
- Validasi APKK-APKR - Elim RantepaoDocument272 pagesValidasi APKK-APKR - Elim RantepaoGARNIS AURORANo ratings yet
- Case Report: Hemophilia ADocument20 pagesCase Report: Hemophilia ABintang Ruth Cecilia FebrinaNo ratings yet
- Case Processing SummaryDocument4 pagesCase Processing SummaryLuthfi LazuardiNo ratings yet
- LEMONGRASS EXTRACT (Cymbopogon Nardus. L) AS PLANT INSECTICIDE AMERICAN COCKROACHES (Periplaneta Americana)Document7 pagesLEMONGRASS EXTRACT (Cymbopogon Nardus. L) AS PLANT INSECTICIDE AMERICAN COCKROACHES (Periplaneta Americana)Moh AdibNo ratings yet
- Perivascular Adipose Tissue 2023 BDocument18 pagesPerivascular Adipose Tissue 2023 Bmiguel contrerasNo ratings yet
- Wards - Units: Main Features of Investigating UnitsDocument6 pagesWards - Units: Main Features of Investigating UnitsErickCarranzaNo ratings yet
- RSUD Jayapura HIV/AIDS ServicesDocument48 pagesRSUD Jayapura HIV/AIDS ServicesStevanus Bob Arvianto AlwieNo ratings yet
- Lab Report InheritanceDocument14 pagesLab Report InheritanceYusri RaemyNo ratings yet
- CCS Heart Failure Guidelines: 2014 Update On New Therapies, Biomarkers, Anemia Management, and Complex CasesDocument88 pagesCCS Heart Failure Guidelines: 2014 Update On New Therapies, Biomarkers, Anemia Management, and Complex CaseseliasNo ratings yet
- CAstV KELong AAAP 2017 PDFDocument16 pagesCAstV KELong AAAP 2017 PDFJimeno Franscisco de los pozosNo ratings yet
- Discount Summary of CentaurusDocument1 pageDiscount Summary of CentaurusAnwarNo ratings yet
- Chenhua Yan, MD: ChinaDocument34 pagesChenhua Yan, MD: ChinaaymenNo ratings yet
- Health Outcomes JAN - JUNE 2022Document2 pagesHealth Outcomes JAN - JUNE 2022Carl TuazonNo ratings yet
- Prevalence of Smear Positive Pulmonary Tuberculosis Among The Workers of Brick Industry of BhaktapurDocument8 pagesPrevalence of Smear Positive Pulmonary Tuberculosis Among The Workers of Brick Industry of Bhaktapurbidur acharyaNo ratings yet
- M. Kiaii Dialyzer Talk-2013Document36 pagesM. Kiaii Dialyzer Talk-2013Komeil RezaeiNo ratings yet
- Jurnal 1Document10 pagesJurnal 1Andi Tri SutrisnoNo ratings yet
- To Study The Visual Outcome and Iop Changes After ND: Yag Laser CapsulotomyDocument5 pagesTo Study The Visual Outcome and Iop Changes After ND: Yag Laser CapsulotomyIJAR JOURNALNo ratings yet
- Gowri BongaigaonDocument32 pagesGowri BongaigaonGowri ShankarNo ratings yet
- MEDCAC Cronenwett PDFDocument37 pagesMEDCAC Cronenwett PDFVladimirTonellodeVasconcelosNo ratings yet
- Chapter Four Result and Findings 4.1: Age of The RespodentDocument13 pagesChapter Four Result and Findings 4.1: Age of The RespodentsareedoNo ratings yet
- Cardio Vascular DiseasesDocument21 pagesCardio Vascular Diseasesvoruganty_vvsNo ratings yet
- Human Papillomavirus Infections: From the Laboratory to Clinical PracticeFrom EverandHuman Papillomavirus Infections: From the Laboratory to Clinical PracticeRating: 5 out of 5 stars5/5 (3)
- Visual Water: An Integration of App and Web to Understand Chemical ElementsDocument5 pagesVisual Water: An Integration of App and Web to Understand Chemical ElementsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Parastomal Hernia: A Case Report, Repaired by Modified Laparascopic Sugarbaker TechniqueDocument2 pagesParastomal Hernia: A Case Report, Repaired by Modified Laparascopic Sugarbaker TechniqueInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Smart Cities: Boosting Economic Growth through Innovation and EfficiencyDocument19 pagesSmart Cities: Boosting Economic Growth through Innovation and EfficiencyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Smart Health Care SystemDocument8 pagesSmart Health Care SystemInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Impact of Silver Nanoparticles Infused in Blood in a Stenosed Artery under the Effect of Magnetic Field Imp. of Silver Nano. Inf. in Blood in a Sten. Art. Under the Eff. of Mag. FieldDocument6 pagesImpact of Silver Nanoparticles Infused in Blood in a Stenosed Artery under the Effect of Magnetic Field Imp. of Silver Nano. Inf. in Blood in a Sten. Art. Under the Eff. of Mag. FieldInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Insights into Nipah Virus: A Review of Epidemiology, Pathogenesis, and Therapeutic AdvancesDocument8 pagesInsights into Nipah Virus: A Review of Epidemiology, Pathogenesis, and Therapeutic AdvancesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- An Analysis on Mental Health Issues among IndividualsDocument6 pagesAn Analysis on Mental Health Issues among IndividualsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Implications of Adnexal Invasions in Primary Extramammary Paget’s Disease: A Systematic ReviewDocument6 pagesImplications of Adnexal Invasions in Primary Extramammary Paget’s Disease: A Systematic ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Compact and Wearable Ventilator System for Enhanced Patient CareDocument4 pagesCompact and Wearable Ventilator System for Enhanced Patient CareInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Relationship between Teacher Reflective Practice and Students Engagement in the Public Elementary SchoolDocument31 pagesThe Relationship between Teacher Reflective Practice and Students Engagement in the Public Elementary SchoolInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Air Quality Index Prediction using Bi-LSTMDocument8 pagesAir Quality Index Prediction using Bi-LSTMInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Predict the Heart Attack Possibilities Using Machine LearningDocument2 pagesPredict the Heart Attack Possibilities Using Machine LearningInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Utilization of Date Palm (Phoenix dactylifera) Leaf Fiber as a Main Component in Making an Improvised Water FilterDocument11 pagesThe Utilization of Date Palm (Phoenix dactylifera) Leaf Fiber as a Main Component in Making an Improvised Water FilterInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Parkinson’s Detection Using Voice Features and Spiral DrawingsDocument5 pagesParkinson’s Detection Using Voice Features and Spiral DrawingsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Investigating Factors Influencing Employee Absenteeism: A Case Study of Secondary Schools in MuscatDocument16 pagesInvestigating Factors Influencing Employee Absenteeism: A Case Study of Secondary Schools in MuscatInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Harnessing Open Innovation for Translating Global Languages into Indian LanuagesDocument7 pagesHarnessing Open Innovation for Translating Global Languages into Indian LanuagesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Exploring the Molecular Docking Interactions between the Polyherbal Formulation Ibadhychooranam and Human Aldose Reductase Enzyme as a Novel Approach for Investigating its Potential Efficacy in Management of CataractDocument7 pagesExploring the Molecular Docking Interactions between the Polyherbal Formulation Ibadhychooranam and Human Aldose Reductase Enzyme as a Novel Approach for Investigating its Potential Efficacy in Management of CataractInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Terracing as an Old-Style Scheme of Soil Water Preservation in Djingliya-Mandara Mountains- CameroonDocument14 pagesTerracing as an Old-Style Scheme of Soil Water Preservation in Djingliya-Mandara Mountains- CameroonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Diabetic Retinopathy Stage Detection Using CNN and Inception V3Document9 pagesDiabetic Retinopathy Stage Detection Using CNN and Inception V3International Journal of Innovative Science and Research TechnologyNo ratings yet
- Dense Wavelength Division Multiplexing (DWDM) in IT Networks: A Leap Beyond Synchronous Digital Hierarchy (SDH)Document2 pagesDense Wavelength Division Multiplexing (DWDM) in IT Networks: A Leap Beyond Synchronous Digital Hierarchy (SDH)International Journal of Innovative Science and Research TechnologyNo ratings yet
- The Making of Object Recognition Eyeglasses for the Visually Impaired using Image AIDocument6 pagesThe Making of Object Recognition Eyeglasses for the Visually Impaired using Image AIInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Electro-Optics Properties of Intact Cocoa Beans based on Near Infrared TechnologyDocument7 pagesElectro-Optics Properties of Intact Cocoa Beans based on Near Infrared TechnologyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Advancing Healthcare Predictions: Harnessing Machine Learning for Accurate Health Index PrognosisDocument8 pagesAdvancing Healthcare Predictions: Harnessing Machine Learning for Accurate Health Index PrognosisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Design, Development and Evaluation of Methi-Shikakai Herbal ShampooDocument8 pagesDesign, Development and Evaluation of Methi-Shikakai Herbal ShampooInternational Journal of Innovative Science and Research Technology100% (3)
- Formulation and Evaluation of Poly Herbal Body ScrubDocument6 pagesFormulation and Evaluation of Poly Herbal Body ScrubInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of Digital Marketing Dimensions on Customer SatisfactionDocument6 pagesThe Impact of Digital Marketing Dimensions on Customer SatisfactionInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Survey of the Plastic Waste used in Paving BlocksDocument4 pagesA Survey of the Plastic Waste used in Paving BlocksInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Comparatively Design and Analyze Elevated Rectangular Water Reservoir with and without Bracing for Different Stagging HeightDocument4 pagesComparatively Design and Analyze Elevated Rectangular Water Reservoir with and without Bracing for Different Stagging HeightInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Auto Encoder Driven Hybrid Pipelines for Image Deblurring using NAFNETDocument6 pagesAuto Encoder Driven Hybrid Pipelines for Image Deblurring using NAFNETInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Cyberbullying: Legal and Ethical Implications, Challenges and Opportunities for Policy DevelopmentDocument7 pagesCyberbullying: Legal and Ethical Implications, Challenges and Opportunities for Policy DevelopmentInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Generic Name:: Norgestimate and Ethinyl EstradiolDocument5 pagesGeneric Name:: Norgestimate and Ethinyl EstradiolJay VillasotoNo ratings yet
- PCCM - Patient-Centered Clinical MethodDocument3 pagesPCCM - Patient-Centered Clinical MethodChidi MbatuegwuNo ratings yet
- Fundamental Concepts of Community Health NursingDocument47 pagesFundamental Concepts of Community Health NursingRhen LiminNo ratings yet
- Visual ImpairmentDocument5 pagesVisual ImpairmentRowly Pearl Iradiel NedicNo ratings yet
- Semen Analysis Guide in 40 CharactersDocument27 pagesSemen Analysis Guide in 40 Charactersangela tanteoNo ratings yet
- Gait Abnormalities Assessment and CausesDocument12 pagesGait Abnormalities Assessment and CausesMudassar SattarNo ratings yet
- Study Guide, Community Health Nursing Science 1Document55 pagesStudy Guide, Community Health Nursing Science 1Enos ErastusNo ratings yet
- Laboratory Diagnostics of (Selected) Endocrine DisordersDocument48 pagesLaboratory Diagnostics of (Selected) Endocrine DisordersPaulina PaskeviciuteNo ratings yet
- Appr MS Id 000563Document7 pagesAppr MS Id 000563LAWSON IYENE-EMINo ratings yet
- Antimicrobial of Monodera MyristicaDocument64 pagesAntimicrobial of Monodera MyristicaUnity EfejeneNo ratings yet
- Use of Local Anesthesia For Pediatric Dental Patients: Latest RevisionDocument6 pagesUse of Local Anesthesia For Pediatric Dental Patients: Latest RevisionzainaNo ratings yet
- Health Education by Kamini MSNDocument15 pagesHealth Education by Kamini MSNkamini Choudhary100% (2)
- Safety and Infection Control: Archer NCLEX Review Crash CourseDocument75 pagesSafety and Infection Control: Archer NCLEX Review Crash CourseDanica Chiara Motia100% (1)
- CDC Growth Charts: United States: KG LB LBDocument1 pageCDC Growth Charts: United States: KG LB LBAlmira ClaraNo ratings yet
- FNCP MaglayaDocument8 pagesFNCP MaglayaVaronNo ratings yet
- Respirologi Makassar Pertemuan IlmiahDocument5 pagesRespirologi Makassar Pertemuan IlmiahMaya Angela LisalNo ratings yet
- Introduction To Pharmacy Practice and Simulation: PHAR456Document82 pagesIntroduction To Pharmacy Practice and Simulation: PHAR456Hassan El HajjNo ratings yet
- Effectiveness of Gallus Gallus Domesticus Eggshells As An Antibacterial Component of Hand SoapDocument71 pagesEffectiveness of Gallus Gallus Domesticus Eggshells As An Antibacterial Component of Hand SoapGabriel Christopher MembrilloNo ratings yet
- StroVac en ITU Recurrente No ComplicadaDocument8 pagesStroVac en ITU Recurrente No ComplicadaCarlos Alberto Aliaga DulantoNo ratings yet
- Therapeutic Modalities 4th Edition Starkey Test BankDocument5 pagesTherapeutic Modalities 4th Edition Starkey Test BankGregoryGreenroyak100% (12)
- Divya Compilation - Gems of PlanetsDocument6 pagesDivya Compilation - Gems of PlanetssourabhNo ratings yet
- POLYCYTHEMIADocument29 pagesPOLYCYTHEMIAFaizan KhanNo ratings yet
- Vojta TherapyDocument4 pagesVojta TherapyPrashu Jain100% (1)
- College of Nursing: Pharmacology Drug StudyDocument2 pagesCollege of Nursing: Pharmacology Drug StudyChristine Pialan SalimbagatNo ratings yet
- 2020thoraxlungs Neckheart VesselsDocument171 pages2020thoraxlungs Neckheart VesselsFaith madayagNo ratings yet