Abstract
Biosimilars offer cost-effective and safe treatment options both for patients and healthcare systems. CT-P10 is the first biosimilar of rituximab approved in Europe for use in all indications of originator rituximab (oRTX). This study aimed to provide real-life data on treatment changes and adverse events in patients who received oRTX or CT-P10. We retrospectively reviewed treatment-related adverse events [infusion-related reactions (IRRs), infections, hypogammaglobulinemia] in patients treated with at least one dose of oRTX (MabThera®) or CT-P10 (Truxima®) between 2020 and 2021 and had at least 6 months follow-up after rituximab infusion in a rheumatology clinic. The switches between oRTX and CT-P10 were performed according to drug availability at the hospital pharmacy at the time of infusion according to the local hospital procedure. Physicians were not involved in the decision of biosimilar selection. A total of 128 patients (CT-P10, n = 64; oRTX, n = 64) were included. CT-P10 was switched in 52 (40.6%) patients who had previously used oRTX, and 48 (37.5%) patients remained on oRTX. We demonstrated no difference between patients treated with oRTX or CT-P10 in the rates of IRRs, in which all reactions were grade 1 and 2. Comparable rates of infections (p > 0.05) and the rate of hypogammaglobulinemia (p > 0.05) were found in both groups with no significant difference. CT-P10 provides a safe treatment alternative in patients who require rituximab therapy. The rational use of biosimilars can be supported by evolving evidence on interchangeability and switching in real-life settings, which will help clinicians in decision-making.
Similar content being viewed by others
Introduction
Biologic agents are breakthrough treatment options for the management of rheumatic diseases. Rituximab is a chimeric monoclonal antibody with a very high molecular weight that shows activity against the CD20 molecule expressed in human B cells. In recent years, it has become one of the standard care options for rheumatic diseases such as ANCA-associated vasculitis (AAV), rheumatoid arthritis (RA), and systemic lupus erythematosus (SLE); however, high cost limits its use in the treatment [1]. Rituximab is also a valuable drug in the treatment of Systemic lupus erythematosus, Systemic sclerosis, Inflammatory myopathies, Sjogren’s syndrome and IgG4-related diseases for the patients who are resistant to conventional agents [2]. Even though it is generally well tolerated, rituximab may cause different types of adverse events, including infusion-related reactions (IRRs), infections, and hypogammaglobulinemia. In particular, IRRs often occur during or after the first rituximab infusion (77%), and the prevalence decreases with subsequent infusions [3].
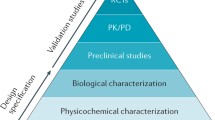
Biosimilars offer safe and cost-effective treatment options for patients and healthcare systems due to increasing healthcare expenditures [4, 5]. CT-P10 is the first biosimilar of rituximab approved in Europe for use in all indications of originator rituximab (oRTX) [6]. The cost of CT-P10 is 60–70% lower than oRTX, providing a significant financial incentive to switch to the use of biosimilars, allowing more patients to access life-saving treatment. One of the problems in biosimilar products including CT-P10 is immunogenicity, which is a major safety issue. It might result in fatal complications by causing unwanted immune responses, which in rare cases, occur as anaphylaxis or hypersensitivity reactions in patients. Immunogenicity data of biosimilar products cannot be directly extrapolated, in particular for large biological molecules such as CT-P10 [7]. Therefore, to accept biosimilars as interchangeable, comparable preclinical and clinical studies must be presented, and it must be shown that the switch from reference drug to biosimilar does not affect patient safety and treatment effectiveness [8]. Indeed, the CT-P10 has been licensed by the European Medicine Agency (EMA) and the Food and Drug Administration (FDA) on the result of data in clinical and preclinical comparability studies in patients with non-Hodgkin lymphoma and RA [9, 10]. Additionally, randomized controlled trials have demonstrated the bioequivalence of CT-P10 and oRTX in terms of efficacy, safety, and immunogenicity, as well as pharmacokinetics and pharmacodynamics properties [11,12,13,14]. Studies on CT-P10 so far indicate that the drug is interchangeable. However, the evaluation of pharmacovigilance issues of biosimilars in a real-world setting, where patient populations typically differ compared to clinical trials, has a significant role in the decision-making process [7]. Until now, real-life studies evaluating the switch from oRTX to CT-P10 in the rheumatic population have included a small number of patients and focused more on effectiveness, but data on safety was quite limited. Therefore, this study aims to describe the real-life experience of CT-P10 use in terms of interchangeability and adverse events in patients with various rheumatic diseases.
Methods
Study protocol and patients
This descriptive study was conducted retrospectively in the University Hospitals Rheumatology Outpatient Clinic and approved by the University Clinical Studies Ethics Committee (KA-22003). Patients aged over 18 years who received at least one dose of oRTX (MabThera®) or CT-P10 (Truxima®) between September 2020 and December 2021 and had at least 6 months follow-up after rituximab infusion were included in the study. According to local hospital procedures, physicians are allowed to use the drug available at the hospital pharmacy at the time of infusion. Therefore, none of the decisions on interchangeable administration was made by the physician her/himself. Originator rituximab or its biosimilar was administered to the patients in real-life circumstances. For the patients with Systemic lupus erythematosus, Systemic sclerosis, Inflammatory myopathies, Sjogren’s syndrome and IgG4-related disease, Rituximab has been used as ‘off label’ after the approval of reimbursements policy.
Clinical evaluation
Data on patients’ demographics, rituximab indication, rituximab infusions (i.e., infusion rate, dose, number of doses), IRRs (i.e., type of reaction, symptomatic treatment of reaction, duration in interruption of infusion), duration of rheumatic disease, concomitant glucocorticoids use, concomitant disease-modifying antirheumatic drugs (DMARDs) use and prior use of DMARDs (conventional or biological) were collected. Premedication therapy consisting of acetaminophen, methylprednisolone, and pheniramine prior to rituximab infusion was standardized to all patients at the same doses. Infusion-related reactions, infections, and rates of hypogammaglobulinemia were assessed as adverse events in the study. The events occurring during the infusion, that is from the beginning to the end of the infusion and within 24 h after the infusion, were considered as IRRs. Data on reactions that occurred within 24 h of the completion of infusion were obtained from patients’ files. IRRs occurred during the infusion were assessed according to the Common Terminology Criteria for Adverse Events (CTCAE); grade 1 events include mild symptoms that do not require intervention, while grade 2 includes moderate symptoms that require interruption of the infusion but responds promptly to symptomatic treatment (e.g., antihistamines). All infections, including requiring hospitalization and/or antibiotics or resulting in disability or death within 6 months after the infusion, were recorded. The IgG, IgA, and IgM levels below the lower limit of normal were evaluated as hypogammaglobulinemia [15].
Statistical analysis
The IBM Statistical Package for Social Science (SPSS, IBM Corp. Released 2015. Armonk, NY: IBM Corp) version 23 program was used for statistical analysis. The variables were investigated using visual (histogram, probability plots) and analytic methods (Kolmogorov–Smirnov, skewness, and kurtosis) to determine whether they are normally distributed or not. Descriptive statistical data were presented as mean, standard deviation (SD), median (interquartile range, (IQR)), numbers, and percentages. Analysis of categorical data of two independent groups was performed using the Chi-square or Fisher exact test. Continuous variables were analyzed using the independent sample t test for parametric variables and the Mann–Whitney U test for non-parametric variables. To identify risk factors associated with IRRs, the variables with p < 0.25 as a result of univariate analysis were included in the multivariate analysis [16]. Factors predicting for IRRs were analyzed by the logistic regression analysis. Data are presented as odds ratios (ORs), with 95% confidence interval (CI) and p value. P values of ≤ 0.05 were considered statistically significant.
Results
Demographic and clinical features
The study included 128 patients (93 female, 35 male) with a mean age (SD) of 53.0 (12.5) years and half of the patients received CT-P10 (Table 1). Fifty-two patients in the CT-P10 group switched to CT-P10 while previously using oRTX (oRTX/CT-P10) due to the procurement policy of the hospital; twelve patients received rituximab infusions for the first time. In patients receiving CT-P10 or oRTX, the most frequent indication for rituximab was RA, followed by AAV and SLE. Median (IQR) disease duration was 8 (10.5) years in CT-P10 group and 9.5 (13.8) years in oRTX group. The patient’s demographics and baseline disease characteristics were similar between groups, except for age, and these data are presented in Table 1.
Rituximab infusions and adverse events
The most common rituximab regimen in both groups was infusions of 1000 mg in a 2-week interval (CT-P10, n = 41 (64%), oRTX n = 40 (62.5%)). The median (IQR) cumulative dose of rituximab was 9 (10.1) g and 10 (11.8) g in CT-P10 and oRTX groups, respectively.
The most common adverse events in this study were IRRs (Fig. 1), with an overall incidence of 43.0% (55 patients). Of those, 25 (grade 1 n = 11, grade 2 n = 14) (39.1%) occurred in the CT-P10, and 30 (grade 1 n = 15, grade 2 n = 15) (46.8%) occurred in the oRTX group (p = 0.372) (Table 2.). Laryngeal paresthesia was the most common form of IRRs in both groups, followed by tightness in the chest and drowsiness/weakness (Table 3). Most IRRs (n = 38, 69.1%) occurred within the first hour of rituximab administration, with a median time of onset was 1 (range, 0.5–3.2) hour. Only 14.5% of IRRs occurred during the first rituximab infusion. In four patients in the oRTX group, and two patients in the CT-P10 group, severe flushing in the face and arms occurred within 24 h after the completion of infusion, which later disappeared spontaneously. All grade 2 IRRs were managed accordingly by temporary interruption of the infusion, administration of paracetamol, methylprednisolone, and/or H1 receptor antagonists, and/or reducing the infusion rate. Discontinuation of the infusion was not required for the management of grade 1 IRRs. No treatment-emergent IRRs of grade 3 or higher were reported in either treatment group. Infections were observed in 19 (33.9%) and 21 (35.0%) patients in the CT-P10 and oRTX groups, respectively (p = 0.903). One patient in the CT-P10 and three patients in the oRTX group had multiple infections. The most frequently reported infections were upper respiratory tract infections (URTIs) and urinary tract infections (UTIs). In each group, six patients required hospitalization due to infections, and three of these infections (two patients and one patient in the CT-P10 and oRTX groups, respectively) resulted in the patient’s death due to COVID pneumonia. Also, most hospitalizations were due to COVID pneumonia (five in each group). Among patients who have data for immunoglobulins levels; in the CT-P10 group, rituximab-induced hypogammaglobulinemia for IgG and IgM were determined in 10 (27.8%) and 11 (44.0%) patients, respectively. In the oRTX group, these rates were 4 (10.5%) and 10 (30.3%), respectively. Infusion details, IRRs characteristics, and adverse event rates, such as hypogammaglobulinemia and infection, were similar in both groups (p > 0.05), summarized in Table 2.
Predictive markers for infusion-related reactions
In our study, many variables such as age, gender, smoking status, disease duration, previous treatments, cumulative rituximab dose, the cycle of rituximab, and duration of infusion were analyzed as predictive markers for IRRs in all patients receiving rituximab. The risk of developing IRRs was not different between patients who received CT-P10 or oRTX [odds ratio (OR) 1.376; 95% confidential interval (CI) 0.68–2.78; p = 0.373]. At univariate analysis, patients who developed IRRs were more frequently females (p = 0.018) and had longer disease duration (p = 0.004), but these factors were found not significant at multivariate analysis (p = 0.099 and p = 0.052, respectively) (Table 4).
Discussion
Our study has explored real-life experiences with the use of originator and biosimilar rituximab in a rheumatology setting. This is the largest study that provides data on interchangeability and safety issues in heterogeneous populations with rheumatologic diseases in a post-marketing real-world setting. The decision on using biosimilar or originator rituximab in this study was determined by local hospital procedures, not by physicians’ personal/professional decisions. The study findings have shown no significant difference between oRTX and CT-P10 groups in terms of adverse events including IRRs, infections, and rituximab-induced hypogammaglobulinemia. Additionally, CT-P10 was shown to be a safe alternative to the originator rituximab. The most frequently reported adverse events were IRRs, with an overall incidence of 43%, with similar proportions of patients in each group (39.1% and 46.8% for oRTX and CT-P10, respectively). These rates are in accordance with previous clinical studies of rituximab, where the incidence of IRRs ranged from 22 to 71% [17,18,19,20]. None of the reactions reported in these studies was considered serious, all resolved without causing any problems, and most occurred after the first infusion and within the first hour of infusion. The IRRs rates observed in phase 3 studies ranged between 15 and 32% for CT-P10 and 9.5–30% for oRTX [10, 12, 21, 22]. Although real-life data are limited in studies with CT-P10, it has been reported that IRRs rates are 16–27% in patients with lymphoma [23, 24], and about 10% in rheumatologic populations [25, 26]. Stubbs et al. indicated that IRRs were observed in 40% and 33% of the CT-P10 and oRTX groups, respectively, in patients with immune-mediated thrombotic thrombocytopenic purpura patients [27]. The relatively higher rate of IRRs in our study can be explained by the inclusion of adverse events, such as a mild degree of burning/itching of the throat or nausea (especially at the beginning of the infusion), where symptomatic treatment is applied. Furthermore, the assessment of patients with various rheumatological diseases in this study may explain the difference in the rates of IRRs found in phase 3 studies conducted on patients with RA. However, all the observed IRRs in our study were grade 1 or grade 2, in accordance with the literature, and were successfully treated with symptomatic treatment, such as intravenous glucocorticoids and antihistamines. Most of these reactions occurred within the first hour of the infusion. However, contrary to the literature, the IRRs observed in this study mainly occurred in the subsequent infusions. This may be explained by the fact that a complete comparison could not be made due to the relatively small number of patients who received the originator or biosimilar rituximab infusion for the first time.
In our study, infection rates including serious infections requiring hospitalization, were comparable between CT-P10 and oRTX groups (33.9% and 35.6%, respectively). The most frequent infections in both groups were URTIs and UTIs. Additionally, hospitalizations due to COVID pneumonia were the most common in both groups. The results reported in our study were very much in line with previous comparative studies of the originator and biosimilar rituximab. In phase studies conducted among patients with rheumatoid arthritis and lymphoma, infections occurred in 22–46% of patients in the oRTX group and 24–50% in the CT-P10 group [10, 12,13,14, 21, 22]. Consistent with our study findings, URTI and UTI were the most frequently reported infections in these studies; however, these rates are lower in studies involving real-life data [15, 23, 25,26,27,28]. In a study of diffuse large B-cell lymphoma patients [23], the overall infection rate with rituximab was 14.5%, while in refractory SLE patients [25], this rate was 18.8%, of which 12.5% included severe infections. In three different studies with CT-P10 among patients with IgG4-related disease [26], AAV [15], and RA [28], infection was observed in approximately 21% of the patients. In patients with immune-mediated thrombotic thrombocytopenic purpura, infective complications (mainly urinary tract infections) were reported in 15% of patients in the oRTX group and 18% in the CT-P10 group [27]. Considering that data were collected during the COVID-19 pandemic for this study, COVID-pneumonia could have an impact on higher occurrence rates of infections compared to previously reported rates. Moreover, it is thought that use of high-dose glucocorticoids or a history of immunosuppressive drugs, such as cyclophosphamide may trigger the risk of infections in some patients which might explain the high incidence of infection in this study.
We demonstrated no significant difference between the oRTX and CT-P10 groups with regards to the development of hypogammaglobulinemia, with rates of 10.5% and 27.8% for IgG and 30.3% and 44.0% for IgM, respectively. These results were in accordance with the previously reported range in the literature [15, 26, 29]. Although the rate of hypogammaglobulinemia was found to be different between the groups, this was not reached a statistical significance due to the assessment of a few numbers of patients whose immunoglobulin levels were measured. Antonelou et al. found that in patients with AAV, hypogammaglobulinemia occurred at 22.8% and 36% for IgG and 34.8% and 28% for IgM in oRTX and CT-P10 groups, respectively [15]. In patients with IgG4-related disease, this rate was 10.5% with CT-P10 [26]. In another study with oRTX among patients with rheumatoid arthritis, 14.8% and 37.9% of patients had IgG and IgM levels below the lower limits of normal, respectively [29].
Two different real-life studies determined various variables that may be associated with the development of IRRs [30, 31]. In the study by Prakash et al. none of the clinical features or laboratory parameters have found to be significantly correlated with the incidence of IRRs with the use of biosimilar rituximab [30]. It was stated that a small number of patients included in the study might be the reason for the lack of significance. In another study with the oRTX in the heterogeneous pediatric population, higher lymphocyte counts were associated with a higher risk for IRRs [31]. In our study, we analyzed particular clinical or laboratory parameters as predictive markers for the development of IRRs in all patients receiving rituximab; the risk was higher in patients with longer disease durations and females in univariate analysis. However, no significance was detected (p = 0.052) in multivariate analysis. Therefore, those findings are needed to be assessed in larger populations and more comprehensive studies in the future.
It is important to note that this study has some limitations. First of all, due to the fact that the study was retrospective, data depended on the accuracy and completeness of medical charts and reports by the physicians. However, regular completion of patients’ anamnesis and detailed rituximab follow-up charts may have somewhat compensated for this deficiency. In addition, subgroup analysis by underlying rheumatological diseases could not be performed due to having a heterogeneous population for diagnosis. Finally, our data’s single-center nature may limit the finding’s generalizability.
Despite the limitations, our study remains the largest to show a comparable safety profile of CT-P10 and the oRTX in rheumatic patients in a post-marketing real-world setting. Our findings have demonstrated that there are no significant differences in adverse events between the originator and the biosimilar rituximab in treating patients with rheumatic disease. Given the value of cost/effectiveness, the use of biosimilars may result in reduced treatment costs, thereby increasing patients’ access to rituximab treatment and providing economic benefits for healthcare systems. Preferences and practices of rheumatologists to use biosimilars depend mainly on the national (or local) regulatory process which is established by the availability of safety data including a large number of patients. Therefore, we believe that an increased number of real-life studies on biosimilars conducted among patients with various diseases could assist healthcare providers, stakeholders, and decision makers in using biosimilar rituximab.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Schioppo T, Ingegnoli F (2017) Current perspective on rituximab in rheumatic diseases. Drug Des Devel Ther 11:2891–2904
Berghen N, Vulsteke JB, Westhovens R, Lenaerts J, De Langhe E (2019) Rituximab in systemic autoimmune rheumatic diseases: indications and practical use. Acta Clin Belg 74(4):272–279
Genentech Inc. Rituxan (rituximab): US prescribing information (2019) Available from: https://www.gene.com/download/pdf/rituxan_prescribing.pdf. Accessed 31 Dec 2021
Cohen HP, Blauvelt A, Rifkin RM, Danese S, Gokhale SB, Woollett G (2018) Switching reference medicines to biosimilars: a systematic literature review of clinical outcomes. Drugs 78(4):463–478
Dorner T, Strand V, Cornes P, Goncalves J, Gulacsi L, Kay J et al (2016) The changing landscape of biosimilars in rheumatology. Ann Rheum Dis 75(6):974–982
Choi D, Lee S, Kim S, Yoon S (2022) A developer’s perspective on clinical evidence and benefits for rituximab biosimilar uptake, with a focus on CT-P10. Clin Drug Investig 42(4):285–300
Biosimilars in the EU, Information guide for healthcare professionals (2019) European Medicines Agency (EMA) and the European Commission (EU), Available from: https://www.ema.europa.eu/en/documents/leaflet/biosimilars-eu-information-guide-healthcare-professionals_en.pdf. Accessed 31 Dec 2021
McKinnon RA, Cook M, Liauw W, Marabani M, Marschner IC, Packer NH et al (2018) Biosimilarity and interchangeability: principles and evidence: a systematic review. BioDrugs 32(1):27–52
Ogura M, Sancho JM, Cho SG, Nakazawa H, Suzumiya J, Tumyan G et al (2018) Efficacy, pharmacokinetics, and safety of the biosimilar CT-P10 in comparison with rituximab in patients with previously untreated low-tumour-burden follicular lymphoma: a randomised, double-blind, parallel-group, phase 3 trial. Lancet Haematol 5(11):e543–e553
Buske C, Jurczak W, Sancho JM, Zhavrid E, Kim JS, Hernandez-Rivas JA et al (2021) Long-term efficacy and safety of CT-P10 or rituximab in untreated advanced follicular lymphoma: a randomized phase 3 study. Blood Adv 5(17):3354–3361
Shim SC, Bozic-Majstorovic L, Berrocal Kasay A, El-Khouri EC, Irazoque-Palazuelos F, Cons Molina FF et al (2019) Efficacy and safety of switching from rituximab to biosimilar CT-P10 in rheumatoid arthritis: 72-week data from a randomized Phase 3 trial. Rheumatology (Oxford) 58(12):2193–2202
Suh CH, Yoo DH, Berrocal Kasay A, Chalouhi El-Khouri E, Cons Molina FF, Shesternya P et al (2019) Long-term efficacy and safety of biosimilar CT-P10 versus innovator rituximab in rheumatoid arthritis: 48-week results from a randomized phase III trial. BioDrugs 33(1):79–91
Yoo DH, Suh CH, Shim SC, Jeka S, Molina FFC, Hrycaj P et al (2017) Efficacy, safety and pharmacokinetics of up to two courses of the rituximab biosimilar CT-P10 versus innovator rituximab in patients with rheumatoid arthritis: results up to week 72 of a phase I randomized controlled trial. BioDrugs 31(4):357–367
Yoo DH, Suh CH, Shim SC, Jeka S, Cons-Molina FF, Hrycaj P et al (2017) A multicentre randomised controlled trial to compare the pharmacokinetics, efficacy and safety of CT-P10 and innovator rituximab in patients with rheumatoid arthritis. Ann Rheum Dis 76(3):566–570
Antonelou M, Abro A, Heath R, Iacovou A, Ashley C, Caplan J et al (2022) Comparison of outcomes using the rituximab originator MabThera with the biosimilar Truxima in patients with ANCA-associated vasculitis. Scand J Rheumatol 51(2):135–141
Zhang Z (2016) Model building strategy for logistic regression: purposeful selection. Ann Transl Med 4(6):111
Cohen SB, Emery P, Greenwald MW, Dougados M, Furie RA, Genovese MC et al (2006) Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum 54(9):2793–2806
Emery P, Fleischmann R, Filipowicz-Sosnowska A, Schechtman J, Szczepanski L, Kavanaugh A et al (2006) The efficacy and safety of rituximab in patients with active rheumatoid arthritis despite methotrexate treatment: results of a phase IIB randomized, double-blind, placebo-controlled, dose-ranging trial. Arthritis Rheum 54(5):1390–1400
MabThera (rituximab) [summary of product characteristics] (2015) London, UK: European Medicines Agency (EMA). Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000165/WC500025821.pdf. Accessed 25 Apr 2022
Emery P, Deodhar A, Rigby WF, Isaacs JD, Combe B, Racewicz AJ et al (2010) Efficacy and safety of different doses and retreatment of rituximab: a randomised, placebo-controlled trial in patients who are biological naive with active rheumatoid arthritis and an inadequate response to methotrexate (Study Evaluating Rituximab’s Efficacy in MTX iNadequate rEsponders (SERENE)). Ann Rheum Dis 69(9):1629–1635
Kwak LW, Sancho JM, Cho SG, Nakazawa H, Suzumiya J, Tumyan G et al (2022) Efficacy and safety of CT-P10 versus rituximab in untreated low-tumor-burden follicular lymphoma: final results of a randomized phase III study. Clin Lymphoma Myeloma Leuk 22(2):89–97
Park W, Bozic-Majstorovic L, Milakovic D, Berrocal Kasay A, El-Khouri EC, Irazoque-Palazuelos F et al (2018) Comparison of biosimilar CT-P10 and innovator rituximab in patients with rheumatoid arthritis: a randomized controlled Phase 3 trial. MAbs 10(6):934–943
Lee K, Ha JY, Jung AR, Lee YS, Lee SW, Ryu JS et al (2020) The clinical outcomes of rituximab biosimilar CT-P10 (Truxima((R))) with CHOP as first-line treatment for patients with diffuse large B-cell lymphoma: real-world experience. Leuk Lymphoma 61(7):1575–1583
McBride A, Daniel S, Driessen MT, Szende A, Choudhry A, Tian M et al (2021) Assessment of rituximab-abbs, a biosimilar, and rituximab outcomes in patients with CLL or NHL: a real-world UK study. Leuk Res 111:106671
Pongtarakulpanit N, Pisitkun P, Ngamjanyaporn P (2020) Efficacy and safety of rituximab biosimilar in refractory lupus. Lupus Sci Med 7(1):e000442
Della-Torre E, Lanzillotta M, Campochiaro C, Di-Colo G, Mancuso G, Capurso G et al (2021) Efficacy and safety of rituximab biosimilar (CT-P10) in IgG4-related disease: an observational prospective open-label cohort study. Eur J Intern Med 84:63–67
Stubbs MJ, Low R, McGuckin S, Newton R, Thomas M, Westwood JP et al (2019) Comparison of Rituximab originator (MabThera) to biosimilar (Truxima) in patients with immune-mediated thrombotic thrombocytopenic purpura. Br J Haematol 185(5):912–917
Cacciapaglia F, Renna D, Fornaro M, Venerito V, Lopalco G, Iannone F (2021) Safety and effectiveness in switching from reference to biosimilar rituximab in rheumatoid arthritis patients: real world experience from a single Italian rheumatology centre. Clin Exp Rheumatol 39(5):1147–1148
van Vollenhoven RF, Fleischmann RM, Furst DE, Lacey S, Lehane PB (2015) Longterm safety of rituximab: final report of the rheumatoid arthritis global clinical trial program over 11 years. J Rheumatol 42(10):1761–1766
Prakash G, Malhotra P, Khadwal A, Lad D, Suri V, Kumari S et al (2018) Infusion related hypersensitivity reactions with bio-similar anti CD-20 monoclonal antibody rituximab in indian patients: a retrospective study. Indian J Hematol Blood Transfus 34(2):273–277
Legeay C, Bittencourt H, Haddad E, Spiesser-Robelet L, Thepot-Seegers V, Therrien RA (2017) Retrospective study on infusion-related reactions to rituximab in a heterogeneous pediatric population. J Pediatr Pharmacol Ther 22(5):369–374
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Author information
Authors and Affiliations
Contributions
MB-K: conceptualization, methodology, investigation, formal analysis, writing—original draft. ED: conceptualization, methodology, resources, investigation, formal analysis, writing—original draft. AB-E: writing—review and editing, visualization, supervision. OK: methodology, writing—review and editing, supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The study was approved by the University Clinical Studies Ethics Committee (KA-22003).
Consent to publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bahap-Kara, M., Duran, E., Bayraktar-Ekincioglu, A. et al. Interchangeability and adverse events in originator-rituximab and its biosimilar (CT-P10) among rheumatic patients: a real-life experience. Intern Emerg Med 18, 791–799 (2023). https://doi.org/10.1007/s11739-023-03222-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03222-x