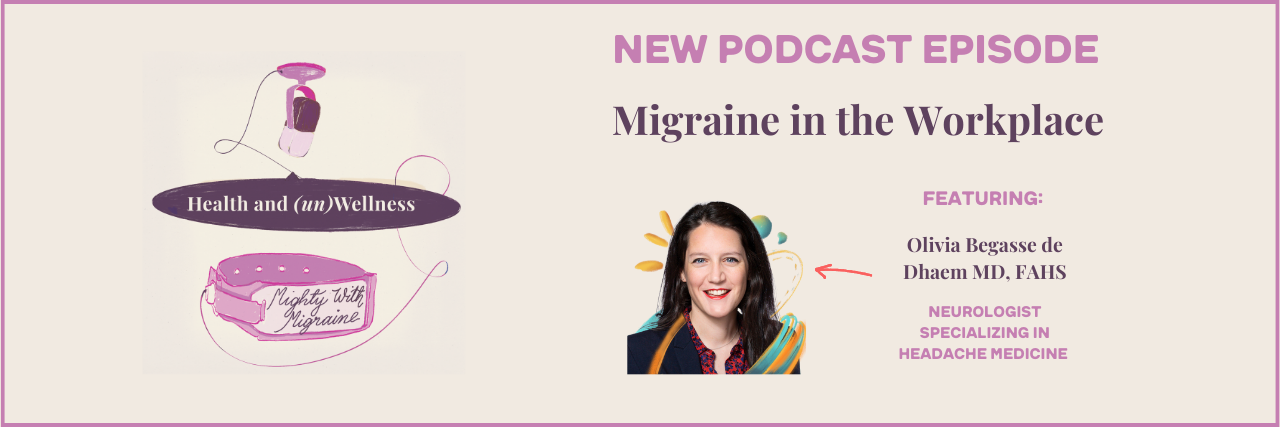
In this week’s venting-sesh-turned-productive conversation, Kat and Skye are joined by headache specialist and executive committee member of the International Headache Society Global Patient Advocacy Coalition (IHS-GPAC), Olivia Begasse de Dhaem MD, FAHS. Together, they discuss why people with migraine struggle to succeed in the workplace (spoiler alert: it’s not them), how others can support them, and tips for requesting individualized accommodations. Oh, and in case you’re curious of the episode’s general vibes: People with migraine want to work, but often can’t due to inaccessible workplaces or lack of flexible career opportunities. Thanks for coming to our TED Talk!
You can also listen on our Spotify for Podcasters page and on Apple Podcasts.
Additional Reading:
Working Full-Time Despite Chronic Illness Does Not Mean I’m ‘OK’
8 Hacks to Help You Get Through the Workday When You Have Migraine
Episode Transcript:
Skye Gailing
Welcome to Health and (un)Wellness.
Kat Harrison
A podcast brought to you by The Mighty, where we put the human back in health. I’m Kat.
Skye Gailing
And I’m Skye, and we are your hosts for this season, Mighty With Migraine.
Kat Harrison
Between the two of us, our heads have over 33 years of experience being a pain in our brains.
Skye Gailing
Yours too? Let’s be friends who wear sunglasses inside.
Kat Harrison
Now on to today’s episode, where we’ll be discussing migraine in the workplace. Hello, Skye.
Skye Gailing
Hello, Kat.
Kat Harrison
We’ve been gearing up for this episode for a while. It’s a topic that we both feel super passionately about and have a lot of real world experience in, though I wish we didn’t. But it feels really unfair to our audience that we know how incredible our special guest is, but they do not! So please, right the wrong and introduce her.
Skye Gailing
It would be my pleasure to introduce everyone to Dr. Olivia Begasse de Dhaem, a neurologist who works as a headache specialist in Connecticut. She is a member of the executive committee of the International Headache Society-Global Patient Advocacy Coalition (aka IHS-GPAC). She’s passionate about advocacy to support people with headache diseases in the workplace. She has written on the topic in scientific journals and in the Harvard Business Review, and has given national and international talks on the topic. She recently co-edited a book for Oxford University Press, “Headache (What Do I Do Now?).” Dr. Olivia, thank you so much for being here.
Dr. Olivia
Thank you so much for having me and for covering such an important topic.
Kat Harrison
It’s a big one! We have been very lucky to have a couple of neurologists on with us this season. And I think one of my favorite questions to ask right at the beginning is not “Why neurology?,” but “Why headache medicine?”. What about that field interests you?
Dr. Olivia
So I initially got into the field of headache medicine to learn more for my mom. I grew up with a mom who’s had chronic migraine for most of her life, without knowing it for most of her life, but with most of the symptoms including significant sensitivity to sound. I couldn’t even wear a watch around her because of the noise of the watch. And she’s so strong, so resilient. But despite everything, that significantly affected her ability to study or work. I remember I was around six years old and I was with her when she sought care. She explained all of her symptoms to the doctor, like sensitivity to lights, sound, noise, nausea, vomiting, difficulty concentrating. So the doctor just said, “Oh, it’s just a headache, take aspirin.” And even though I was six, it felt so wrong. So when I was in med school and residency, I really wanted to do electives to learn more about headache medicine, but then you meet people with headache diseases and are like, “Oh, I just love these people. I want to join the team.” I’ve been so impressed by all the resilient people with headache disease. And now, it’s more fun because we have more treatment too. A lot of these treatments help a significant number of people. It’s always nice to see people come back with a smile because migraine got better and their lives too as a result.
Kat Harrison
I hope to one day be a smiling migraine patient. How about you, Skye?
Skye Gailing
Not smiling just yet, but hopefully one day.
Kat Harrison
One day. It’s something to aim for. The reason why you are today’s guest for today’s episode is that you have a research focus and particular interest in the intersection of migraine in the workplace. I’m very curious how that became the intersection that interests you.
Dr. Olivia
It just breaks my heart to see really hard-working, brilliant people not achieve their professional dream and potential because of the disease and the stigma associated with the disease. Early in my training, I met a brilliant man who could speak so many languages, was so cultured, and I asked him what he does for work and he said, “I work as an Uber driver.” And then talking more about it, he said that he used to work as an international lawyer and had to change jobs because his migraine attacks were associated with difficulty speaking, so clearly he couldn’t do his job with his migraine attacks. So that’s when I felt like this is more than seeing one patient after the other and prescribing treatment. I think we have to get out there, outside of the clinic, and also try to advocate. You cannot advocate without data, so then you need research. So then that’s the research part about the workplace.
Kat Harrison
I feel like, Skye, a misconception in the world at large — not just about chronic illness and not just about migraine — but this concept that people who live with health conditions don’t want to work. I see Olivia in our recording studio raising her hands like “yes! yes!”, but it’s this wild idea that not everyone wants to contribute to society, that we don’t want to have value, that we don’t want to have purpose. Not that having a job is the pinnacle of existence, but we want to work, we want to thrive, we want to be out there. I actually asked our community this, Skye, and the results are devastating. What were they?
Skye Gailing
They’re relatable, but like you said, devastating. So we asked our community, “Have you ever had to leave a job or school because of your health?” And 51% of the people who responded said, “Yes, they’d had to leave a job.” 10% said, “Yes, they’d had to leave school.” 19% said, “Yes, they had to leave both at some point due to their health,” and only 7% said that they’ve never had to leave work or school for health reasons. And I know I’ve had to leave different jobs for health reasons. How about you, Kat? Do you have experience with this?
Kat Harrison
So much. There’s a lot of factors at play here, right? When we talk about migraine in the workplace, is it: Are you physically able to work? Do you have a position, a company, a culture that is accessible? That provides accommodations? Are you at a point in your treatment journey where you literally can work, whether it’s at home or in the office? I think there are a couple of things that are happening here. Olivia, would you say those results roundabout fit what you see in your patients?
Dr. Olivia
I mean, for my patients, it’s a little bit worse in a sense because once you make it to the headache clinic [your quality of life is likely lower]. I see a biased population, so the numbers are even higher that I see, I would say. But to your first point about people wanting to work — right now we talk about issues studying and working, but people are going to work at the expense of their personal life, self-care, childcare, social life. People with migraine or headache diseases — and I’m sure other chronic diseases and pain are the same — but people are going to prioritize their work at the expense of anything else in their life, to which I think should be counted. But what you say also goes along the way of The Migraine Impact Report from Eli Lilly and The Migraine Association of Ireland survey too. About 70 to 80% of people with migraine have an impact on their professional life because of migraine, but 55% of people had to change their current scores because of migraine, and even people who are active in the workforce, about 40% of people are led to miss out on work opportunities, promotion, increase earning potential, because of migraine.
Kat Harrison
Well, I think I pretty much fit into each of those categories. What you said first is probably my biggest level of experience, which is that I have to prioritize work — and it comes at the expense of everything else in my life. So sometimes I get the question of, “Kat, you must be doing OK, considering you can work full time.” And it’s like, I work full time because it’s the thing I pour my energy into most, but you haven’t seen the state of my kitchen, you haven’t seen what my laundry pile looks like, you haven’t seen the fact that like I haven’t really seen my friends in months, maybe years. And I think it’s that exchange of what you have to give in order to get what you need from work, that’s a huge component of it. Skye, I’m curious, you had a really interesting story about when you first saw the intersection of, say, school and accommodations and migraine, I would love to hear it.
Skye Gailing
Yeah, I mean, I had no idea that it was even possible to have accommodations for migraine, which sounds kind of ridiculous saying it out loud. But I’ve been living with migraine since I was 13. When I was 19, I was in my sociocultural anthropology class and I had just turned in my accommodations paperwork, because I had accommodations for anxiety and panic attacks. And then somebody else turned in her paperwork and she was like, “Yeah, my accommodation is that when I feel the migraine attack coming on, I can get up and leave the class and go lay down.” I was like, “What? That’s a possibility?” I’ve just been sitting there, you know, at the time the abortive medication I was taking was a nasal spray so I would just be hunched over my backpack taking my nasal spray in the middle of class because nobody ever was like, “Hey, this is a chronic condition that you got to take care of. Put yourself first, not last, silly.” That really blew my mind because I was like, “Oh, you can try to explain what you’re going through to people?”. And I think that was also a turning point for me for taking the fact that I do live with migraine seriously. At the time, too, I was working a very physically demanding job while going to class full time. That wasn’t great for pain of any kind. So I started to take my health more seriously when I saw that it was possible and, in fact, encouraged to.
Kat Harrison
Let’s take a quick break to change our shades and then get back at it.
Ubrelvy Migraine Mid Roll
Hi, I’m Ali Raisman. I’ve been living with migraine for a while. As an athlete and gymnast I was taught to just power through the pain. Now I use Ubrelvy or Ubrogepant to treat my migraine attacks. As soon as I feel a migraine attack, I take Ubrelvy, which provides me with quick relief. Once I get relief, I go on with my day. I’m partnering with Ubrelvy to share my migraine story.
Ubrelvy quickly stops migraine in its tracks within two hours without worrying where you are. Most people had pain relief and some even had pain freedom within two hours. Ubrelvy treats migraine attacks in adults and is not for prevention. It’s available by prescription only. Do not take with strong CYP3A4 inhibitors or if allergic to Ubrelvy. Allergic reactions can happen and may occur hours to days after use — get medical help right away if you have swelling of the face, mouth, tongue, or throat or trouble breathing. The most common side effects were nausea and sleepiness.
My hope is that by sharing my migraine story, and the relief I get from Ubrelvy, it can help someone else. Ask your doctor about Ubrelvy, the anytime, anywhere migraine medicine. Find more product information at Ubrelvy.com or call 8444-UBRELVY. Sponsored by AbbVie.
Skye Gailing
…and we’re back!
Kat Harrison
I have reached a point in my career where I cannot work in person. If I want to have any sort of semblance of quality of life, I have to work from home. And I think that that’s taught me that with the right job, with the right situation, it’s very possible for the talented people that live with migraine to have a fulfilling career. I feel like that kind of feeds into the narrative of “Well, I have migraine or I have a chronic illness and I guess I have to do this.” And I think that part of it is, yeah, sometimes you are relegated; you’re kind of put in the corner like “well, this is all I can get.” And then I think the other thing that I would say to any employers or managers out there is that you’re missing out on a really, really great candidate pool. There are a bunch of people out there who are so talented, and also just bring a lot of diverse and inclusive experience. I’m not sure if you see that as well, Olivia, when you talk with patients?
Dr. Olivia
Yes, people have to get creative. And thank you both for sharing those powerful stories, I’m sure a lot of people can relate to them. And migraine is extremely isolating, because there’s a stigma. And because of the symptoms, you push through your workday and at the end, people just want to lay down in a dark room — quiet, no screen, nothing, right? So it’s so isolating because of so many reasons, then the information doesn’t get out there. It’s not talked about enough and I’m glad we are working to change that. I also think people don’t know the possibilities of work. That’s why we’re trying to change things because I see a lot of people who have such a discrepancy between the initial dream and what they’re doing now because of the impact on their studies and then on their work. And hopefully we can raise awareness even for younger people so we can make a change early on.
Kat Harrison
Work is a part of our identity in ways that are both good and bad, right? Like I really, really like talking to people about health. I love creating conversations. I love being an advocate. I did not realize that this was a possibility for me early in my career. I started my career in magazine editorial, which was an absolute bucket list, dream job. So thrilled with myself that I was able to do it, but it got to the point where I could not sustain that lifestyle. I was working 9- to 10-hour days, going to events at night. I had events on the weekend and I was like, “This would be a lot even for someone that doesn’t live with the condition.” But I have some level of headache every single day. And I was pushing through and then I had to spend months in bed. That’s the only way I saw myself, and so it took over a decade for me to really step back and see who else can I be, what can I bring to the table, and so a lot of it is that internalized ableism that we talk a lot about, Skye, is how you perceive yourself. What do you think you’re capable of? And I think getting creative, I think that that’s the key — we put professionalism in a box. We want work to look like a square. But really work is shapeless or it should be, right? Think of the world and growing technology. I wish it wasn’t so rigid. Do you feel like rigidity, Skye, has really played into your experience?
Skye Gailing
Oh yeah, it’s a lot of black-or-white thinking. I thought in part because I had amazing educators and people who supported me, but I was like, “Oh, they say I’m capable of doing this. I should do whatever they say” — not even give it a second thought. If you asked six years ago what I’d be doing, I’d be like, “Oh yeah, I’m gonna be on this international archaeology dig. Probably leading it, working on my PhD.” I thought I was gonna do that and then somehow act and tap dance on the side. That is not what I’m doing now.
Kat Harrison
Would love to see the tap dancing though, Skye!
Skye Gailing
I miss it. I miss it. My joints, not what they once were for archaeology digs or tap dancing. But yeah, I really thought my life would look very different. I thought I’d be in Italy right now or something by this point in my life. So when I knew that that couldn’t happen, or that wasn’t going to happen… yes, there’s the grief of chronic illness. But there’s also that grief of losing the identity or losing the future you thought you were going to have. I’m going to be 27 in a few months and I just saw so many people I went to school with getting their master’s degrees, getting married, having kids, like doing all this stuff. And I’m like, “Oh, what is my path? What is my career?” It’s not what I thought it was gonna be. It’s not what I told everybody else it was going to be. Where do I go from here? And it’s the rigidity of, “Oh, well, if you don’t have your career, you’re not a productive member of society” or things like that. All these lies we are fed really played a harmful part of my journey,
Kat Harrison
And you don’t know what you don’t know. Olivia, where I really try to step back and say — but if you’ve never lived with migraine, if you didn’t grow up with a parent with migraine, if you didn’t realize that the sound of a watch could set off an attack, how does the workplace change? So, you were part of a very interesting research study about migraine and work and I would love to hear more about it and what you’ve learned.
Dr. Olivia
I think there’s a huge part here of internalized stigma, and then people have different feelings like grief, shame, guilt, and that actually by itself is associated with lower productivity. So there’s really the disease on the limitation of the disease itself, but a big part is an issue with stigma and lack of understanding, even some recognition acknowledgement in the workplace.
So the Fujitsu Headache Project was done in collaboration with the International Headache Society, Global Patient Advocacy Coalition (IHS-GPAC), and Fujitsu, an information technology company and the health promotion team. So it is our first large-scale headache education and evaluation program in the workplace. So really, the goal was to educate the entire employee population based in Japan, including supervisors, managers, more than 73,000 of employees. 91% of the employee population of Fujitsu in Japan participated in the program, and that’s really the key, it’s hard to do. But it’s key if you’re trying to make a change. So, with huge participation, they found that about 17% of people had migraine, but 77% had some headache. As a result of participation in the education program, 73% of participants said that their understanding of headache diseases improved, and 83% of people without headaches said that their behavior toward a colleague with headache disease changed. And that’s really part of the goal here. Those who wanted a consultation with a headache specialist, they could be seen, and for those with moderate to severe headaches, it increased productivity by 1.5 days of decreased absences from employees per year. And then 14 days of increased productivity per employee per year. So the study had a two-fold positive return on investment.
Kat Harrison
Hear that everyone? Hear that all the leadership out there? Those numbers are mind-blowing, when you think about the number of people who live with some type of headache disorder or actually have a migraine diagnosis. That’s a lot of people. You are actually able to make some type of a change. And I think the education part is such a huge component of this.
Skye Gailing
Yeah, those numbers are incredible. It gives me hope, because there was that willingness to learn more and the study turned out well. And I think that goes to show that accessibility can be as basic as educating everybody on what a headache disorder is or what migraine looks like in the workplace. Like Kat was saying before, we want to work, we just need to be met where we’re at and that can come through accommodations or increased accessibility. We asked our site about this too. We said, “In your opinion, is your workplace or school accessible for people who live with migraine?”. And 50% of people voted for “No, if anything, it’s harmful.” Only 5% of respondents said it’s fully accessible — so, a long way to go for us to be more like Fujitsu.
Kat Harrison
So one thing you had told us when we were doing our tech check, Olivia, was didn’t you ask people [at Fujitsu] what word they associated with migraine?
Dr. Olivia
Yes. So, we cannot fully compare Japan to the U.S. because there are a lot of cultural and societal differences, but we can learn from each other, right? And I think two keys about Fujitsu is a top-down approach, like the leadership was fully supportive. And then that’s a company with a lot of health promotion plans, and campaigns, and programs — and the employees are used to health promotion plans in a sense. But when employees were asked, “What is the first word you think of when you hear migraine?,” the most common word was “weather change,” which I would be interested to ask this in the U.S.
Kat Harrison
Oh, well it’s almost like they’ve been listening to this podcast because I’m pretty sure episode number one was just a rant from Skye and I about how much we hate barometric pressure changes! So I would say “weather,” but also I’m pleasantly surprised by that word because I think that sometimes I get too inside myself where I think people would say “annoying” or “painful”…eh, that’s pretty accurate! So I think that “weather”… I find that really fascinating. I want to make sure we get in enough time here. If someone wants to make an accommodation, if someone wants to ask their boss or manager or leadership for something, what are some accommodations that you have seen work from your patients or out in the field?
Dr. Olivia
Maybe I’m biased because I like to have this conversation. But I think it’s important to first have the conversation with your health care providers, or friends, colleagues, or your own support group to really take a step back and think about what are the migraine or headache disease symptoms, frequency, severity, what is the job function — everybody’s different. So for it to really work it has to be adapted to the person, to the disease, and then to the job function, or to the job environment, because sometimes I’ve been impressed by what can be done. I have a patient, she works as a cashier, and I’m talking with the supervisor because I’m feeling stuck… working as a cashier [with migraine]? I mean, everything — the lights, the noise, the posture, everything, right? What can we do? And then they accommodated a closet for her where she could lay down in the dark and take breaks. So, everything has to be individualized. I think it’s knowing your rights, knowing you have a right to reasonable accommodation. Then really having sought beforehand the job functions and what you’re asking.
Kat Harrison
I want to cry. The fact that you talked to one of your patient’s employers about how to better accommodate their job… I can’t even get my providers to talk to each other, I’m currently in a battle to literally get EKG results shipped between them. And also, way to go for your patient! You’re right — such an overstimulating environment in the grocery store, there is a reason why I try to get as much stuff delivered to my house as possible. But like, having an accessible closet? Amazing in the sense that she has a place to go, so just wanted to call that out.
Dr. Olivia
Thank you. It’s a little bit tricky, right? Because we are not trained as headache specialists… we are not trained in that. So sometimes I don’t even know how to get creative because I don’t fully understand the work environment. Everyone works so many different jobs. So I think it’s important to really think, and also migraine is so complicated, with so many implications, it has a lot of emotional impact. So that’s why it’s important to go prepared with the facts about migraine, and then an actual plan to show that as the best result and and if we can have a letter or form from your health care provider, that’s also helpful. But in general, natural lights, sound-free environment, noise reduction, access to water, restroom, good air quality, regular breaks, flexible schedule whenever possible, if possible, changing to non-night shift for people, as you alluded to, whenever possible, remote work helps a lot of people. And in general, living in a good supportive work environment is very important. And then a sense of autonomy and job satisfaction — they’ve also been associated with increased migraine-related productivity.
Kat Harrison
Skye, what’s the one workplace accommodation that’s made the biggest difference for your migraine?
Skye Gailing
Being able to work remotely, but also being able to work asynchronously sometimes has really helped. I mean, yesterday, I had a real doozy of an attack. And I ended up working for like 20 minutes and then I had to log off for an hour and just lay down in the dark. And I was able to do that and then returned to work. I’ve never been able to do that anywhere else because I’ve worked in person otherwise, and that’s made the biggest difference in my ability to work.
Kat Harrison
I think that that is probably mine as well. That was the game-changer for me. I also think we have created a culture here at The Mighty, and I would really love to see others adopt it, where we don’t really try to schedule meetings too late in the day. We have a group of us who have chronic illnesses, and I don’t know about you, Skye — in fact, I do know about you because we’re very similar this way — which is as the day goes on, I just become a shell of myself. Like you said, Olivia, you work all day, you push yourself, and at the end of the day you flop onto the couch. So asking me to have a 4 p.m. EST meeting, it’s not going to go very well, you’re not going to get my best work. So I think accommodating schedules that way, and just absolutely zero hardships from managers about going to doctor’s appointments. We go as frequently as we need to, we go whenever we need to during the day; the amount of stress, the amount of time off I used to have to take from my very small bank of PTO, having to provide a doctor’s note. I really hope for the most part, though, we’ve gotten past that whole: “I’m out today.” “Where’s your doctor’s note?” That’s a very antiquated, ableist practice we have here.
I want to talk for 10 more hours, but I am very sad because I hear people don’t like 10-hour podcasts. Olivia, thank you so much for joining us today and sharing your expertise. We really appreciate it.
Dr. Olivia
Thank you so much for having me on and all your wisdom about the topic. I hope it helps a lot of people.
Skye Gailing
Thank you so, so much for being here. Dr. Olivia, are there any resources you want to recommend?
Dr. Olivia
So for resources, the International Headache Society Global Patient Advocacy Coalition (IHS-GPAC) has a website. I really like the resources of the American Migraine Foundation and they have a wonderful Facebook support group, Move Against Migraine.
Skye Gailing
So, Dr. Olivia, your book “Headache (What Do I Do Now?” from Oxford University Press, can you tell our listeners a bit about what it’s about?
Dr. Olivia
Yes — surprise! — headache. But it’s a concise practical case space book that goes through different headache diagnoses to really help people and practitioners in the clinic as they see patients, as a resource to help with easy diagnosis or all the other options and treatment.
Skye Gailing
That’s amazing. I’m so excited for it.
Kat Harrison
Who’s the readership of that?
Dr. Olivia
It’s mostly targeted for any provider interested in headache medicine, because it’s really hard to just sit down and read a textbook that’s really focused on what has to be done right then. So hopefully it helps people as they see people with headache disease without being overwhelmed. My book is available on Amazon and on Oxford University Press.
Skye Gailing
Great. Thank you so much. I will definitely be visiting every single website right after this. Thank you so much for being here. Thank you, Kat, for being spectacular as always.
Kat Harrison
Right back at you.
Skye Gailing
Thank you so much everyone out there for listening. We hope you laughed and learned in equal measure, and that your head is kind to you today.
Kat Harrison
Join us on our next episode, where we will be talking about having a social life — or not! — with migraine.
Skye Gailing
No pressure to bring your best self, just your authentic one.
Kat Harrison
Because we’re here for you, in sickness and in health. Download The Mighty app for more.